Introduction
Endovascular Aneurysm Repair (EVAR) has been the modality of choice for elective Abdominal Aortic Aneurysms (AAA)
for over 30 years [1] owing to its shorter operating length, decreased length of stay, invasive nature compared to Open Surgical Repair (OSR), physician and patient preference [2-7], and
immediate morbidity and mortality benefits [3]. However, Type
Annals of Surgical
Case Reports & Images
II Endoleaks (T2Es), defined as retrograde collateral blood flow
into the aneurysm sac from the lumbar or Inferior Mesenteric
Artery (IMA), are a common complication, occurring in 16%-
50% of EVARs [2,8]. The course of T2Es varies significantly, and
many resolve spontaneously. Others persist but do not cause
significant sac enlargement, whereas others continue to grow
with or without intervention. While many retrospective studies have been conducted in the last 30 years in larger institutions and academic centers in the United States and Europe, the
consensus on treating persistent T2Es with increasing sac size
varies, especially among community-based vascular surgeons.
However, there is now a consensus regarding the treatment of
all type II endoleaks when sac enlargement exceeds 5 mm in a
6-month interval [4]. It is common to attempt to resolve them
with minimally invasive measures initially and to reserve surgical conversion in refractory cases when the aneurysm grows
too large, becomes symptomatic, and there is an unacceptable
risk of rupture. Newer techniques, such as transcaval or translumbar embolization, have shown promising results. However,
standardized training in fellowship programs has been developing slowly. Herein, we present a case in which standard transarterial embolization failed. Without other techniques at our
disposal, we provided the patient with the option of another
attempt at the transarterial approach or open conversion. He
opted for the latter but may have benefited from a newer endovascular approach.
Case presentation
A 70-year-old male with several comorbidities (stable essential hypertension, dyslipidemia on chronic statin therapy, CKD
III, GERD, COPD with pulmonary blebs, and a history of spontaneous pneumothorax) presented to the vascular clinic for a
routine follow-up visit for an enlarging AAA despite a previous
EVAR. He initially underwent EVAR with bilateral accessory renal artery embolizations for a 5.8 cm AAA on 12/01/2016. Accessory renal embolization was performed due to the large size
(>4 mm) of the arteries. A small, delayed type II endoleak was
observed and presumed to be retrograde flow from the lumbar
arteries. The endoleak continued to be present on subsequent
CT angiography over the next two years, but with a minimal
increase in sac size (6.0 cm). Although the patient remained
asymptomatic, there was sufficient concern he was still at an
unsatisfactory risk of sac rupture, and a decision was made to
perform direct angiography and coil embolization of the lumbar
arteries and aneurysm sac. However, these treatments are not
always curative in nature. The patient was monitored bi-annually with US and non-contrast CT because of concerns regarding contrast nephropathy. There continued to be progressive
growth of the aneurysm sac on this imaging until it reached 7.0
cm in April 2021 (1.2 cm change over 4.5 years) and was confirmed on CTA, where there appeared to be a small endoleak
from the IMA. At this point, the patient was given the option
of an angiogram with coil embolization of the IMA vs. open exploration of the AAA sac with ligation of the bleeding source
and possible graft explantation, and chose the latter. Other approaches were not used in our toolkit and were not offered.
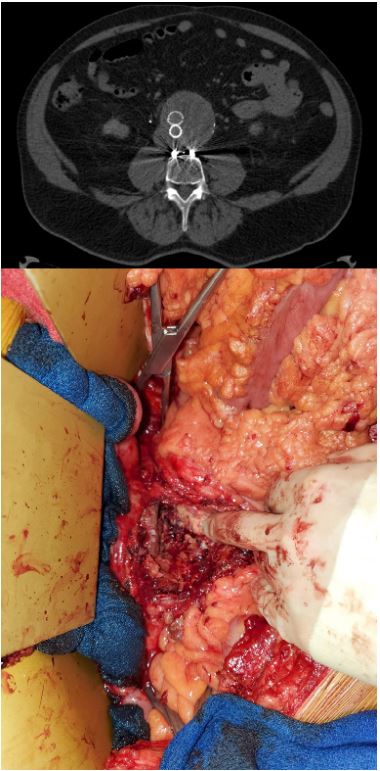
Surgery was performed shortly after using the transperitoneal
approach because of the surgeon’s preference without a significant issue. The aorta and iliac vessels were dissected, and
the loops were placed in preparation for sacotomy. However,
there was no pulsation of the aneurysm; therefore, the aorta
was not clamped before the incision into the sac. After a significant amount of thrombus was removed, vigorous bleeding
was noted from the IMA and the left accessory renal artery, and
each was ligated with a 2-0 silk oversewn suture.
Additionally, bleeding from the lumbar artery was observed,
although to a much lesser degree, it was still oversewn. No
further bleeding was noted prior to sac closure, and the endograft did not appear to have any structural or functional issues.
Hemostatic agents were placed, and the sac was closed watertight with a Prolene suture in a running-locked fashion.
Discussion
T2Es are an unavoidable problem after EVAR. Many patients
do not require interventions; however, this is not always the
case. However, consensus on the treatment of persistent leaks
with an enlarged aneurysm sac remains unclear. Furthermore,
newer minimally invasive techniques, such as the transcaval or
translumbar approaches, have shown promising results in small
case studies and systematic reviews but are less impressive in
others [9-16].
In our patient, transarterial embolization was attempted
but ultimately failed, and we did not initially push for other interventions. However, our patient became concerned with
the aneurysm’s increasing size to approximately 1 cm over two
years after embolization. The patient was given the option of
another transarterial embolization attempt or open conversion,
which he preferred to undergo. In part, his decision was made
because he wanted a procedure that he was assured would be
definitive and had become tired of the imaging and surveillance
processes. Other procedures, such as the transcaval and translumbar approaches, may have been better follow-up approaches because of their less invasive nature and high success rates
[16-18]. However, anatomical considerations, specialized equipment, and training in these techniques are needed and are reserved for academic or larger institutions. The industry has begun to offer specialized courses to learn these procedures but at
the physician’s time and expense. If these treatments continue
to be useful in managing T2Es, the vascular surgical community should emphasize exposure and instruction earlier in their
training.
Although our patient has performed well with his treatment,
our eventual open conversion negates the advantages of EVAR.
While there is no clear consensus on the modality of choice in
these situations, much of the literature suggests that attempting at least one transarterial intervention before considering
others is prudent [19,20]. If this fails, which is not uncommon,
safer, and minimally invasive (endovascular) options with adequate success rates would benefit vascular surgeons.
Conclusion
Given the current technology available, T2Es that require intervention due to an enlarged sac size will continue to be an
issue, given the frequency of EVAR. Many techniques are available and well described in the literature, with newer approaches such as transcaval and translumbar, as viable alternatives to
transarterial or open repair. Although OC, as shown in our case,
remains reliable and definitive, effective endovascular solutions
are the preferred approach under many circumstances. However, more structured training and experience are needed during
fellowships and for practicing vascular surgeons.
Declarations
Data access statement: Data supporting this study are included in the article and/or supporting materials.
Funding statement: No funding was received for this study.
Research: This work was conducted under the supervision
of Stephen Smith MD as a case study under no formal organization.
Ethical compliance: All procedures performed in this study
involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest: The authors declare that they have no
affiliations with or involvement in any organization or entity
with any financial interests in the subject matter or materials
discussed in this manuscript.
References
- Carpenter JP, Baum RA, Barker CF, Golden MA, Mitchell ME, et al. Impact of exclusion criteria on patient selection for endovascular abdominal aortic aneurysm repair. J. Vasc. Surg. 2001; 34: 1050-1054.
- Bryce Y, Schiro B, Cooper K, Ganguli S, Khayat M, et al. Type II endoleaks: Diagnosis and treatment algorithm. Cardiovasc Diagn Ther. 2018; 8(Suppl 1): S131-S137. doi: 10.21037/cdt.2017.08.06.
- Malas M, Arhuidese I, Qazi U, et al. Perioperative mortality following repair of abdominal aortic aneurysms: Application of a randomized clinical trial to real-world practice using a validated nationwide data set. JAMA Surg 2014;149:1260-5.
- Moll FL, Powell JT, Fraedrich G, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European Society for Vascular Surgery. Eur J Vasc Endovasc Surg. 2011; 41(suppl 1): S1-S58. doi: 10.1016/j.ejvs.2010.09.011.
- Columbo J, Martinez-Camblor P, O’Malley A, Suckow B, Hoel A, et al. Long-term Reintervention after Endovascular Abdominal Aortic Aneurysm Repair. Annals of Surgery. 2021; 274 (1): 179-185. doi: 10.1097/SLA.0000000000003446.
- Reise JA, Sheldon H, Earnshaw J, Naylor AR, Dick F, et al. Patient Preference for Surgical Method of Abdominal Aortic Aneurysm Repair: Postal Survey. Eur. J. Vasc. Endovasc. Surg. 2010; 39: 55-61.
- James McAndrew Jones BA, Yiyuan David Hu BA, Mark Anthony Eid MD, Catherine J, Sensenig BA, et al. Short-Term Concerns Primarily Determine Patient Preference for Abdominal Aortic Aneurysm Repair. Journal of Surgical Research. 2022; 269: 119-128.
- D A Sidloff, PW Stather, E Choke, M J Bown, R D Sayers. Type II endoleak after endovascular aneurysm repair. British Journal of Surgery. 2013; 100: 1262-1270.
- Rae S Rokosh, Winona W Wu A, Ronald L Dalman, Elliot L Chaikof. Society for Vascular Surgery implementation of clinical practice guidelines for patients with an abdominal aortic aneurysm: Endoleak management.
- M Ferrari SG, Sardella R, Berchiolli D, Adami C, Vignali V, et al. Surgical Treatment of Persistent Type 2 Endoleaks, with Increase of the Aneurysm Sac: Indications and Technical Notes. Eur J Vasc Endovasc Surg. 2005; 29.
- Joy Walker, Lue-Yen Tucke, Philip Goodney, Leah Candell, Hong Hua, et al. Type II endoleak with or without intervention after endovascular aortic aneurysm repair does not change aneurysm-related outcomes despite sac growth. J Vasc Surg. 2015; 62: 551-61.
- Sana Mulay, Anna CM, Geraedts Mark, JW Koelemay, Ron Balm. ODYSSEUS study group. Type 2 Endoleak With or Without Intervention and Survival after Endovascular Aneurysm Repair. Eur J Vasc Endovasc Surg. 2021; 61: 779e786.
- DA Sidloff, PW Stather, E Choke, MJ Bown, RD Sayers. Type II endoleak after endovascular aneurysm repair. British Journal of Surgery. 2013; 100: 1262-1270.
- Nicola Mangialardi, Sonia Ronchey, Matteo Orrico, Eugenia Serrao, Vittorio Alberti, et al. Surgical conversion with graft salvage as a definitive treatment for persistent type II endoleak causing sac enlargement. J Vasc Surg. 2015; 62: 1437-41.
- Julien Dié Loucou, Lucie Salomon du Mont, Aline Jazayeri, Anne Sophie Mariet, Mélanie eboffe, et al. Evaluation of the Effectiveness of Endovascular Treatment of Type 2 Endoleaks. Annals of Vascular Surgery. 2023; 93: 9-17.
- Giancarlo Mansueto, Daniela Cenzi, Mirko DOnofrio, Enrico Petrella, Andrew A. Gumbs, Roberto Pozzi Mucelli. Treatment of Type II Endoleaks after Endovascular Repair of Abdominal Aortic Aneurysms: Transcaval Approach. Cardiovasc Intervent Radiol.2005; 28: 641-645.
- Terhi Nevala Æ Fausto Biancari Æ Hannu Manninen Æ PekkaSakari Aho Æ Pekka Matsi Æ Kimmo Ma¨kinen Æ Wolf-Dieter Roth Æ Kari Ylo¨nen Æ Mauri Lepa¨ntalo Æ Jukka Pera¨la.
- Caroline G, Burley Mark H Kumar, Waseem A Bhatti, Christina Boyd, Clifford M, et al. Transcaval embolization is the preferred approach. J Vasc Surg. 2019; 69: 1309-13.
- Petroula Nana, Konstantinos Spanos, Franziska Heidemann, Giuseppe Panuccio, George Kouvelos, et al. Systematic review on transcaval embolization for type II endoleak after endovascular aortic aneurysm repair. Journal of Vascular Surgery. 2022; 76(1): 282-291.
- Trans lumbar Embolization of Type II Endoleaks. 12 Years of Experience at a Regional Vascular CentreWiliam Rhodri Thomas, Salil Karkhanis, Jonathan Hopkins, and Martin Duddy Vascular and Endovascular Surgery. 2020; 54(5): 389-394.
- George A Antoniou, Stavros A, Antoniou, Francesco Torella. Editor’s Choice - Endovascular vs. Open Repair for Abdominal Aortic Aneurysm: Systematic Review and Meta-analysis of Updated Peri-operative and Long-Term Data of Randomised Controlled Trials, European Journal of Vascular and Endovascular Surgery. 2020; 59(3): 385-397.
- The Lancet, Open versus endovascular repair of aortic aneurysms, The Lancet. 2020; 95(10230): 1090.