Introduction
Warty Dyskeratoma (WD), alternatively is referred to as isolated Darier disease or focal acantholytic dyskeratosis, is an infrequent mucocutaneous anomaly [1]. Generally, it appears as a
solitary, asymptomatic umbilicated papule, commonly observed
in the head and neck area of individuals in the middle to older
age group [2]. There has been a slight predisposition towards
males that has been identified. Occasional reports have indicated the presence of involvement in the oral and vaginal mucosa
[3,4]. When observed within the oral cavity, WD is predominantly observed on the hard palate and alveolar ridge [5]. The
Annals of Surgical
Case Reports & Images
etiology of Oral Warty Dyskeratoma (OWD) remains unknown,
although a majority of cases have demonstrated a correlation
with tobacco smoking/chewing, local chronic trauma/irritation
caused by a sharp tooth, or an improperly fitted denture [6].
A disease known as warty dyskeratoma exhibits morphologic
traits that resemble those of the typical viral wart, potentially
indicating a connection to Human Papillomavirus (HPV) infection as an underlying cause.
Currently, there is a lack of comprehensive research investigating the possible role of HPV infection in the development of
these lesions. Recently, there have been notable instances of WD that have histological similarities to HPV-induced verrucous
lesions. This observation indicates a broader range of morphological variations in this lesion than previously acknowledged,
and suggests a potential association with HPV infection as an
etiological factor [7]. Currently, there is no evidence of HPV-associated oral warty dyskeratomas in the existing literature, and
none of the documented cases have experienced a recurrence
[8].
This study thoroughly analyses a case of oral warty dyskeratoma occurring in the same patient at distinct locations and
at different times. This is the first report of warty dyskeratoma
thought to be linked with HPV in a current collection of literature.
Case presentation and result
Patient 68-year-old male patient first presented to Gazi University Faculty of Dentistry, Department of Oral and Maxillofacial Surgery in 2018 for evaluation of a white lesion in the left
retromolar region. The patient reported that he did not have any
systemic disease, did not take any medication regularly, and did
not have any skin lesions. In the anamnesis, it was discovered
that the patient had been smoking around 30 cigarettes per day
for a period of 40 years. No abnormalities were observed during the assessment of the extraoral examination. Intraoral examination revealed a white lesion in the left retromolar region,
which was white, erythematous in some areas and did not go
away with scraping. The preliminary diagnosis of the lesions
were oral papilloma, oral leukoplakia, and oral squamous cell
carcinoma. The lesion was surgically excised. To obtain a conclusive diagnosis, the sample was preserved in a solution of 10%
buffered formalin and then transported to the Oral Pathology
Department at Gazi University for histologic investigation. Macroscopically, the lesion was observed as an off-white mucosal
tissue with an irregular surface measuring 1.5x1.3x1 cm in size.
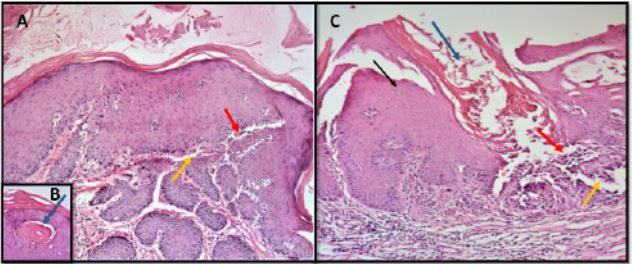
Histopathologically, invaginations and verrucous extensions on
the surface of orthokeratinized epithelium as well as suprabasilar separation and keratin plug were observed. Small groups of
individual keratinocytes were seen in the areas of basilar separation in the lesions. The final diagnosis reported by the pathology department was oral warty dyskeratoma (Figure 1).
Although no recurrence was expected after total excision,
the same patient presented to Gazi University Oral, Dental and
Maxillofacial Surgery in 2022 for examination of a white lesion
on the right palatinal mucosa. Upon intraoral examination, a
firm and white plaque was observed on the right hard palate,
which was resistant to removal with scraping. The histopathologic analysis showed a halo appearance in the cytoplasm of
keratinocytes in the spinous layer of the epithelium, along with
the results of the lesion in the retromolar region in the second
biopsy. Therefore, the presence of HPV was suspected in second biopsy, and PCR analysis was performed to investigate the
presence of HPV.
The potential presence of HPV was hypothesised based on
histochemical staining, and further molecular tests were conducted to determine the presence of HPV-DNA. Formalin-Fixed
Paraffin Embedded (FFPE) tissue samples were cut into 5 sections of 10-micron thickness and taken into ependorf tubes. After deparaffinization, DNA extraction was performed using FFPE
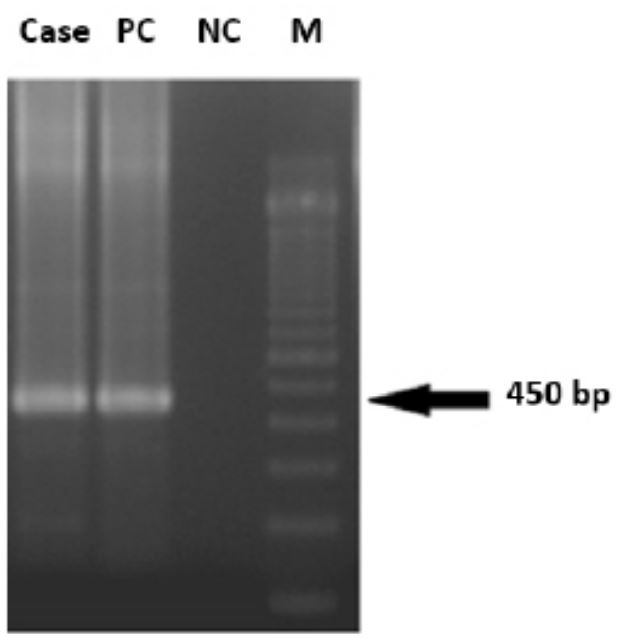
DNA isolation kit (Qiagen, Germany), following the manufacturer’s instructions. PCR was conducted after isolating the sample,
utilising the MY09/MY11 primer combination to amplify the
HPV location. PCR studies were conducted with a negative control containing a PCR mixture without DNA, and the patient material with known HPV presence was used as a positive control.
Ten microliters of the PCR product were loaded onto a 2% agarose gel for gel electrophoresis. The gel was then stained with
ethidium bromide at a concentration of 500 ng/ml in 1x TBE
buffer solution. A GeneRuler DNA ladder (Thermo Scientific in
Vilnius, Lithuania) was utilised as a molecular weight standard.
The analysis yielded a band indicative of the presence of HPV,
which was observed at the 450bp region (Figure 2). With the
molecular data and histopathologic data observed in this study,
the final diagnosis reported by the pathology department was
HPV-associated warty dyskeratoma.
Discussion
WD is considered to be a skin lesion of relatively low prevalence. OWD is commonly encountered on keratinized mucosa,
such as the maxillary and mandibular alveolar ridges and the
hard palate [1]. Tobacco and alcohol intake have been identified
as the most prevalent risk factors connected with OWD [8]. This
study documented a case of OWD occurring in the retromolar
region and on the right side of the hard palate, with a time gap
of 4 years in the same patient. It was noticed that the patient
had a longstanding habit of smoking.
OWD can be categorized as a verruco-papillary lesion based
on its clinical appearance. In some cases, a relatively smooth
surface in the form of papules or patches was seen. It was observed that in certain instances, the surface was rather smooth
and took the appearance of papules or patches. The lesion appears white because to the hyper-keratinization of the surface
epithelium. When a white patch is present, the color white and
the related tobacco habits frequently result in a provisional diagnosis of leukoplakia. In the case of a rough surface, it may
indicate verrucous carcinoma/verrucous hyperplasia or Oral
Squamous Cell Cancer (OSCC) [8].
Despite being a non-progressive minor lesion, it often needs
further investigation due to its clinical and histopathologic
similarities With Oral Potentially Malignant Diseases (OPMDs)
and OSCC [9]. During the diagnostic process, it is essential to
do histopathologic examination in order to distinguish OWD
from other lesions that may have similar characteristics. Leukoplakia is a term used to describe a lesion that appears as a
white patch, particularly when there is a history of tobacco use.
In instances of this nature, the lack of epithelial dysplasia, the
existence of suprabasal clefting, the presence of keratin-filled
crypts, and the occurrence of acantholytic dyskeratotic cells
(known as corps ronds and grains) would serve as the differentiating characteristics from tobacco-induced possibly malignant
leukoplakic lesions [9]. Warty dyskeratoma can be differentiated from Squamous Cell Carcinoma (SCC) based on its histological characteristics, despite its similar verruciform appearance and chronic ulceration. Notably, warty dyskeratoma lacks
atypia or mitotic activity [10]. In contrast to OSCC, the OWD is
characterized by its inherent self-limiting nature and absence of
malignant progression. In instances of this sort, the disparity in
size may serve as a significant signal of the characteristics of the
lesion. The majority of instances of OWD are smaller than 1 cm
in size and exhibit a distinct and clearly defined boundary [11].
The term “wart” suggests that the lesion typically has a surface
that is rough and bumpy, resembling warts. Thus, the typical
clinical differential diagnosis includes Verrucous Hyperplasia
(VH), Verrucous Carcinoma (VC). Unlike VC and VH, OWD is selflimiting and does not lead to malignant change. OWD is clearly
delineated, unlike locally invasive lesions such as VC, VH [8].
The majority of prior descriptions mostly focus on individual
case reports or small series. Thus far, there have been only a
limited number of comprehensive clinicopathologic studies
conducted [12,13]. The etiology and classification of warty
dyskeratoma remain uncertain. Numerous writers claim that
various external variables or a contagious viral pathogen could
potentially play a role in the development of these lesions. However, earlier studies have failed to support these hypotheses or
provide any substantiated proof of a viral infection in relation
to these lesions [14]. The histopathological characteristics of
WD, particularly the striking similarity between cystic lesions
and verrucous lesions, led us to investigate the potential association between HPV infection and the development of these
lesions [7]. While previous reports have shown that focal oral
warty dyskeratomas do not exhibit recurrence, our case study,
as documented by Kaugars (1984) [5], presents evidence to the
contrary. Specifically, we noticed a recurrence in our instance
after a period of 4 years. In order to investigate this particular
issue, Kaddu et al. (2002) [7] conducted a polymerase chain reaction analysis to detect the presence of HPV DNA in 13 lesions
of WD. The results of their study did not reveal any indication of
HPV DNA. However, in our study supported by PCR, we demonstrated the presence of HPV in warty dyskeratoma.
Rushiti et al. (2023) [15] found that HPV-associated oral mucosal lesions exhibited an average recurrence period of 1 year.
No cases of recurrent OWD were found in previous studies and
the presence of HPV was not detected in any of these studies.
Taken together, this may suggest the possibility that the identification of HPV and the observation of multifocal recurrence in
our case are related. It is necessary to conduct sequence studies
on biopsies taken from patients who have experienced a recurrence in order to confirm this concept. The answer to whether
the presence of HPV promotes recurrence or whether the presence of HPV in a multifocal area is connected with HPV can only
be found in this circumstance.
Declarations
Data availability statement: The data supporting the findings of this study are available upon request from the corresponding author. The data were not publicly available because of privacy or ethical restrictions.
Acknowledgements: I would like to thank Tübitak ULAKBIM
for providing project and publication support.
Conflict of interest: The authors declare that they have no
conflicts of interest.
Fundıng: This study was not funded by an organization.
Informed consent form: Informed consent was obtained
from the participant included in the study.
References
- Allon I, Buchner A. Warty dyskeratoma/focal acantholytic dyskeratosis--an update on a rare oral lesion. J Oral Pathol Med. 2012; 41(3): 261-7. doi: 10.1111/j.1600-0714.2011.01082.x.
- Peters SM, Roll KS, Philipone EM, Yoon AJ. Oral warty dyskeratoma of the retromolar trigone: An unusual presentation of a rare lesion. JAAD Case Rep. 2017; 3(4): 336-8. doi: 10.1016/j.jdcr.2017.04.014.
- Gorlin RJ, Peterson WC, Jr. Warty dyskeratoma. A note concerning its occurrence on the oral mucosa. Arch Dermatol. 1967; 95(3): 292-3. doi: 10.1001/archderm.95.3.292.
- Duray PH, Merino MJ, Axiotis C. Warty dyskeratoma of the vulva. Int J Gynecol Pathol. 1983; 2(3): 286-93. doi: 10.1097/00004347-198303000-00006.
- Kaugars GE, Lieb RJ, Abbey LM. Focal oral warty dyskeratoma. Int J Dermatol. 1984; 23(2): 123-30. doi: 10.1111/j.1365-4362.1984.tb05686.x.
- Allon I, Buchner A. Warty dyskeratoma/focal acantholytic dyskeratosis–An update on a rare oral lesion. Journal of oral pathology & medicine. 2012; 41(3): 261-7.
- Kaddu S, Dong H, Mayer G, Kerl H, Cerroni L. Warty dyskeratoma-follicular dyskeratoma: Analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002; 47(3): 423-8. doi: 10.1067/mjd.2002.122756.
- Raj AT, Awan KH, Patil S, Morgan P, Warnakulasuriya S. Oral Warty Dyskeratoma-A Systematic Review of the Literature. Diagnostics. 2022;12(5):1273.
- Steele JC, Dutton AR, Triantafyllou A, Rajlawat BP. Warty dyskeratoma of the buccal mucosa. Oral Surgery. 2014; 7(4): 236-8. doi: https://doi.org/10.1111/ors.12081.
- Chau MN, Radden BG. Oral warty dyskeratoma. J Oral Pathol. 1984; 13(5): 546-56. doi: 10.1111/j.1600-0714.1984.tb01455.x.
- Patil S, Warnakulasuriya S, Raj T, Sanketh DS, Rao RS. Exophytic oral verrucous hyperplasia: a new entity. J Investig Clin Dent. 2016; 7(4): 417-23. doi: 10.1111/jicd.12166.
- Graham JH, Helwig EB. Isolated dyskeratosis follicularis. AMA Arch Derm. 1958; 77(4): 377-89. doi: 10.1001/archderm.1958.01560040001001.
- Tanay A, Mehregan AH. Warty dyskeratoma. Dermatologica. 1969; 138(3): 155-64. doi: 10.1159/000253979.
- Ackerman AB. Focal acantholytic dyskeratosis. Arch Dermatol. 1972; 106(5): 702-6.
- Rushiti A, Castellani C, Cerrato A, Fedrigo M, Sbricoli L, et al. The Follow-Up Necessity in Human Papilloma Virus-Positive vs. Human Papilloma Virus-Negative Oral Mucosal Lesions: A Retrospective Study. J Clin Med. 2023; 13(1). Epub 20231221. doi: 10.3390/jcm13010058.