Background
Liposarcomas are malignant tumors of mesenchymal origin
that typically occur in the lower limbs and retroperitoneum [1].
They account for 20% of all soft tissue sarcomas, making them
the most common subtype [2]. Primary liposarcoma of the mediastinum, however, is rare, constituting only 0.1-0.75% of all
mediastinal tumors and 2% of all liposarcomas [1,3]. These tumors are slow growing and are typically found incidentally on
imaging or after they have grown large enough to cause compressive symptoms, such as dyspnea, chest pain, hoarseness,
tachypnea, wheezing, and/or superior vena cava syndrome
[3,4]. Surgical resection is the mainstay of treatment for all liposarcomas, though tumor grade correlates with prognosis and
the aggressiveness of the disease. The role of adjuvant chemo immuno- and radiotherapy is not well established. In this article, we present the case of a giant primary mediastinal liposarcoma that was successfully removed via surgical resection.
Case presentation
A 77-year-old undoctored male began experiencing shortness of breath at rest while on vacation in the Philippines. He
saw a physician there who obtained a Chest X-Ray (CXR) and
Computed Tomography (CT) scan which revealed a large mass
in the anterior mediastinum. The patient was advised to undergo biopsy of the mass, so the patient returned to the United States for continued workup and management. He arrived
at our emergency department shortly after his return. At this
time, the patient reported 2 weeks of shortness of breath, most
notable when sleeping or lying flat, that was relieved by turning onto his right side. He endorsed an occasional cough with
no sputum production or hemoptysis. The patient had no history of fever, chills, chest pain, palpitations, difficulty swallowing, nausea, vomiting, abdominal pain, numbness, tingling, or
weakness in the bilateral upper extremities. The patient did
not have any medical history at the time of presentation, but
later established care within our institution and was diagnosed
with hypertension and hyperlipidemia. His family history was
non-contributory. Vital signs were notable for a blood pressure
elevated to 167/82, but otherwise were within normal limits.
Physical examination was unremarkable with regular heart
sounds and clear lung fields bilaterally. Laboratory results were
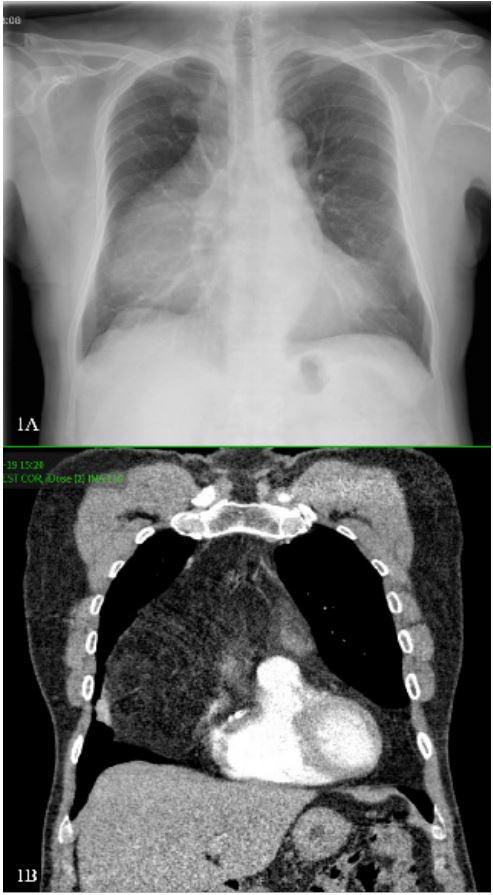
also unremarkable. CXR revealed a large soft tissue mass projected over the right middle and lower hemithorax (Figure 1A).
CT chest with contrast showed a large right anterior mediastinal
mass measuring 15.6 x 8.9 x 16.6 cm consisting of mostly fat
density. The mass appeared mostly well-defined and abutted
the anterior pericardium, ascending aorta, aortic arch vessels,
superior vena cava (SVC), and anterior trachea. The right middle
and lower lobes had mild compressive atelectasis. The differential diagnosis based on this image included liposarcoma, thymolipoma, and teratoma (Figure 1B). The X-ray and CT obtained in
the Philippines were the patient’s first images of the chest, so
no earlier comparison images were available.
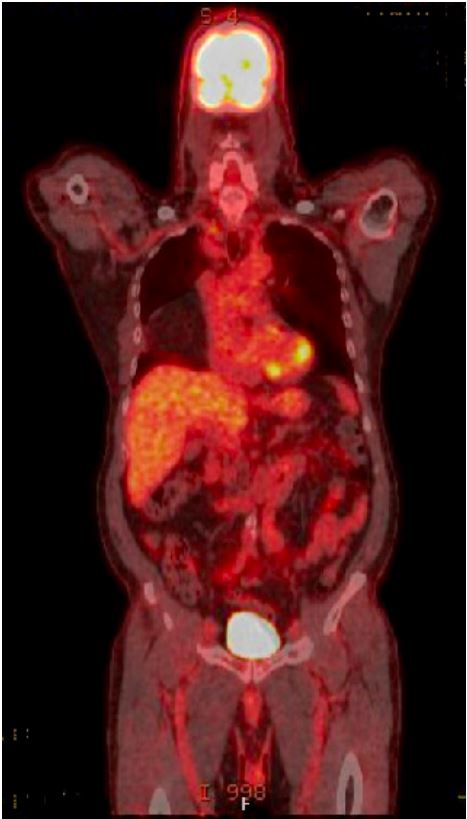
A PET/CT was obtained which re-demonstrated the anterior
mediastinal mass consisting of mostly fat. The mass was mildly
FDG avid (1.8 SUV). It also showed other incidental findings
unrelated to the liposarcoma (Figure 2). Based on the PET/CT
findings an image-guided biopsy of the mediastinal mass was
performed with interventional radiology which revealed an
atypical lipomatous tumor versus a well differentiated liposarcoma. Immunohistochemical stains for CD34, PAX-8, AE1/AE3,
and SOX-13 were all negative.
Complete resection of the mass and total mediastinal exenteration was performed via median sternotomy under general
anesthesia three months after his initial presentation in the
emergency room. The tumor was well-encapsulated and took
up the entire anterior mediastinum, expanding into bilateral
hemithoraces with more significant expansion on the right side.
The pericardium, aorta, and great vessels were easily swept off
and not involved with the mass. Given the size of the mass, an
extensive resection of all the anterior mediastinal structures including thymectomy was done. The dissection extended up into
the neck to the level of the thyroid gland and into both pleural
spaces. The operation was performed without complications
and about 200 cc of blood loss. Surgical pathology confirmed a grade 1 well-differentiated liposarcoma measuring 34 x 28.7 x
10.5 cm. One level 5 lymph node was negative for malignancy.
The tumor was characterized as American Joint Committee on
Cancer (AJCC) stage 1B (pT4 N0). Florescence in situ hybridization (FISH) analysis showed MDM2 gene amplification.
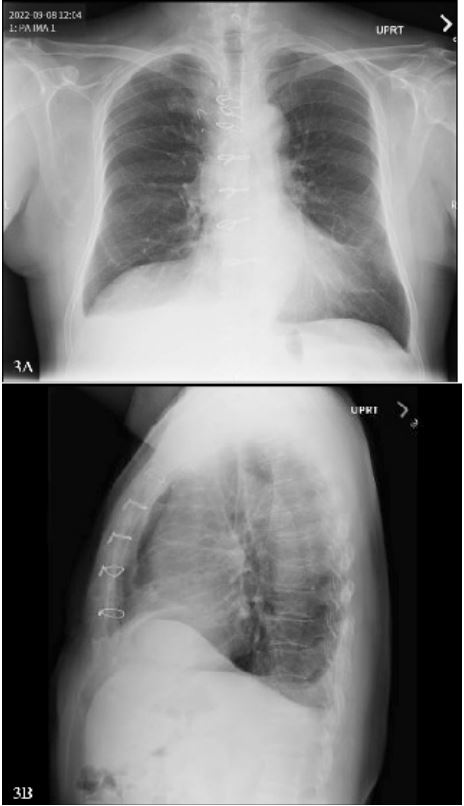
The inpatient postoperative course was unremarkable. CXR
taken two weeks post-operatively showed elevation of the right
hemithorax and mediastinal postoperative changes consistent
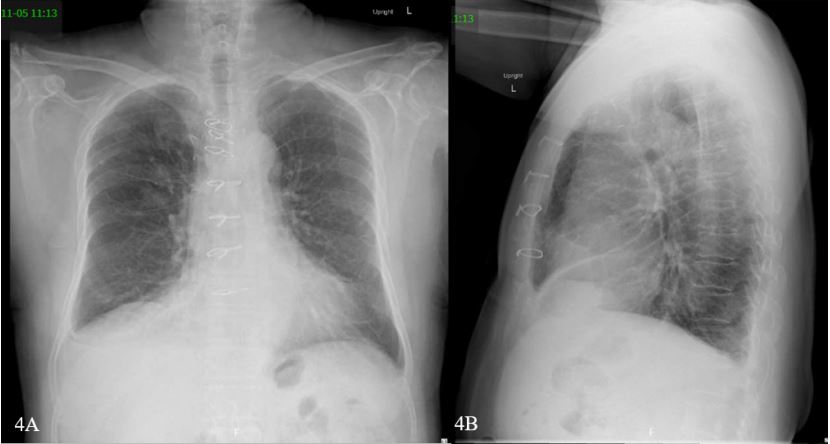
with inpatient CXRs (Figure 3). These findings were unchanged
at two months after surgery (Figure 4). The patient followed up
with medical oncology who did not recommend adjuvant radiation therapy or systemic chemotherapy. Given the low-grade
nature of his tumor, adjuvant therapy was unlikely to pose any
benefit. The patient continues to be closely followed as an outpatient with imaging every 6 months and has had no evidence
of recurrence since his surgery around one year ago.
Discussion
Liposarcomas are derived from primitive mesenchymal cells.
There are four histologic subtypes- well-differentiated, dedifferentiated, myxoid, and pleomorphic- with well-differentiated
being the most common [4-7]. Well-differentiated and atypical
lipomatous tumors carry the best prognosis, whereas pleomorphic and myxoid tend to be more aggressive and carry worse
prognoses. Amplification of the MDM2, CDK4, and HMGA2
genes have been found in both well-differentiated/atypical lipomatous tumors and dedifferentiated liposarcomas [8]. Most
mediastinal liposarcomas develop in the posterior mediastinum,
accounting for almost half of all cases [9]. The next most common location is the anterior-superior mediastinum, followed by
the middle mediastinum, then other locations. There is some
evidence to suggest that well-differentiated and atypical lipomatous liposarcomas occur more frequently in the anterior mediastinum in contrast to the overall tendency for liposarcomas
to originate in the posterior mediastinum [7,9].
The average age at presentation for primary liposarcomas is
50 years old, with a range of 20 to 70 years [10-12]. These tumors grow slowly and generally only produce symptoms once
they have reached a large enough size to compress nearby intrathoracic structures [1,4]. This pattern of growth is thought
be related to these tumors tendency to grow circumferentially
rather than infiltratively [13]. It is estimated that 85% of cases
present with compressive symptoms, whereas the other 15%
of cases are incidentally found on imaging [14]. A review done
by Schweitzer and Aguam found that 63% of patients with mediastinal liposarcomas present with respiratory symptoms, 50%
with chest pain, and 15% with SVC obstruction [15]. The presenting symptoms often mimic common diseases of the heart
and lungs, so obtaining imaging is critical in creating a proper
differential early in the diagnostic workup.
Surgical resection alone is the gold standard of treatment for
mediastinal liposarcomas and is often curative [12,16-18]. Surgical debulking can provide symptomatic relief if complete resection of the tumor is not possible. The role for adjuvant radiation and chemotherapy is not well established for mediastinal
liposarcomas, with some evidence suggesting minimal responsiveness to these treatments and other authors recommending adjuvant radiation be reserved for unresectable and poorly
differentiated tumors [10-12,17]. One case report showed
improvement in long-term survival by five years or more with
use of adjuvant radiation therapy after a partial resection [19].
However, further evidence is needed to establish a clear role for
adjuvant treatments.
Histologic subtype is the best prognostic factor for liposarcomas [12,17]. Tumor size, gender, and age have not been shown
to influence survival [17]. The rates of recurrence for primary
mediastinal liposarcomas range from 10% to 50%, and recurrence can occur years after the initial resection [3,12,17,20]. As
such, close and long-term follow up is recommended for patients with mediastinal liposarcomas, particularly those with
incomplete resections and unfavorable histologic subtypes.
Surgical approach and optimization of risk reduction must
be considered on a case-by-case basis. In the case of large liposarcomas, measures should be taken between the surgical
and anesthesia team to minimize the risk of mediastinal mass
syndrome- a life-threating, acute cardiorespiratory decompensation that can occur with administration of general anesthesia
in patients with large compressive tumors [21,22]. In terms of surgical approach, median sternotomy is most commonly performed, though posterolateral thoracotomy, classic or hemiclamshell thoracotomy can be utilized in certain cases [12].
Smaller tumors that are found incidentally could be resected via
robot-assisted or video-assisted thoracoscopic surgery, but this
is generally not indicated for any tumor exceeding 10 cm [23].
Median sternotomy provides a wide surgical field, allowing for
good exposure of the heart, bilateral lungs, and hilar structures.
A hemi-clamshell incision can expand on this midline approach
to allow better visibility of the lower lobes and posterior hilum.
The most common vascular structure resected in these cases is
the SVC, followed by the innominate vein [24]. SVC involvement
has occurred in multiple cases of primary mediastinal liposarcomas and can be managed with partial SVC resection or complete resection with reconstruction [23].
Conclusion
Primary liposarcomas of the mediastinum are rare tumors
that grow slowly and often present as incidental imaging findings or with compressive symptoms. The primary treatment of
these tumors is surgical resection, typically via median sternotomy, with limited evidence on the role of adjuvant chemotherapy and radiotherapy. Liposarcomas have a high tendency to recur and often recur years after initial surgery, so close long-term
follow up is imperative for these patients. Our patient continues
to be disease free one year after surgery and will continue to be
followed closely with serial imaging.
Declarations
Acknowledgements: No acknowledgements.
Ethics guidelines: Not applicable.
Conflict of interest: No conflicts of interest among any participating authors
Consent for publication: Written informed consent for
publication of their clinical details and/or clinical images was
obtained from the patient/parent/guardian/relative of the patient. A copy of the consent form is available for review by the
Editor of this journal.
References
- Fernández-Tena A, López-González FJ. Mediastinal liposarcoma in a 30-year-old woman with dyspnea and chest pain. Respir Med Case Rep. 2017; 21: 86-88. doi:10.1016/j.rmcr.2017.04.003.
- Lee ATJ, Thway K, Huang PH, Jones RL. Clinical and Molecular Spectrum of Liposarcoma. J Clin Oncol Off J Am Soc Clin Oncol. 2018; 36(2): 151-159. doi:10.1200/JCO.2017.74.9598.
- Wong GS, Bass D, Chen IY, Thomas R, Velez MJ, et al. Imaging and Clinical Findings in a Series of Six Cases of Rare Primary Mediastinal Liposarcoma. Radiol Cardiothorac Imaging. 2022; 4(2): e210259. doi:10.1148/ryct.210259.
- Mani VR, Ofikwu G, Safavi A. Surgical resection of a giant primary liposarcoma of the anterior mediastinum. J Surg Case Rep. 2015; 2015(9): rjv126. doi:10.1093/jscr/rjv126.
- Hahn HP, Fletcher CDM. Primary mediastinal liposarcoma: Clinicopathologic analysis of 24 cases. Am J Surg Pathol. 2007; 31(12): 1868-1874. doi:10.1097/PAS.0b013e318093f925.
- Klimstra DS, Moran CA, Perino G, Koss MN, et al. Liposarcoma of the anterior mediastinum and thymus. A clinicopathologic study of 28 cases. Am J Surg Pathol. 1995; 19(7): 782-791. doi:10.1097/00000478-199507000-00006.
- Suster DI, Suster S. Liposarcomas of the mediastinum. Mediastinum Hong Kong China. 2020; 4: 27. doi:10.21037/med-20-42.
- Dei Tos AP. Liposarcomas: Diagnostic pitfalls and new insights. Histopathology. 2014; 64(1): 38-52. doi:10.1111/his.12311.
- Mediastinal Liposarcoma: Case Report and Literature Review. Accessed. 2023. https://www.scirp.org/journal/paperinformation.aspx?paperid=108852.
- Chen M, Yang J, Zhu L, Zhou C, Zhao H. Primary intrathoracic liposarcoma: A clinicopathologic study and prognostic analysis of 23 cases. J Cardiothorac Surg. 2014; 9(1): 119. doi:10.1186/1749-8090-9-119.
- Raghavan R, Raghuram P, Parekh PV, Kurien JM. Posterior mediastinal liposarcoma simulating a lung mass: An unusual case report. Cancer Imaging. 2007; 7(1): 141-144. doi:10.1102/1470-7330.2007.0021.
- Chen G, Qiu X, Liu Y, et al. Primary mediastinal pleomorphic liposarcoma involving the superior vena cava. Thorac Cancer. 2014; 5(3): 265-270. doi:10.1111/1759-7714.12084.
- Caraglia M, Montella L, Addeo R, et al. Conditions suggesting lymphoma: Case 2. Mediastinal liposarcoma in a patient with previous testicular cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2005; 23(16): 3844-3846. doi:10.1200/JCO.2005.05.056.
- Gaikwad NM, Srikrishna SV, Srikanth K. A rare case of a giant anterior mediastinal liposarcoma. Indian J Thorac Cardiovasc Surg. 2020; 36(2): 148-150. doi:10.1007/s12055-019-00871-6.
- Schweitzer DL, Aguam AS. Primary liposarcoma of the mediastinum. Report of a case and review of the literature. J Thorac Cardiovasc Surg. 1977; 74(1): 83-97.
- Keita P, Tran A, Cheema M, Peterman NJ, Katigbak M. Mediastinal Liposarcoma with Anterior and Posterior Mediastinal Involvement: A Thoracic Oncovascular Case Report. Cureus. 2022; 14(7). doi:10.7759/cureus.26513.
- Yang YS, Bai CY, Li ZC, Li WJ, Li Y. Giant primary liposarcoma of the anterior mediastinum: A case report. Medicine (Baltimore). 2018; 97(42): e12873. doi:10.1097/MD.0000000000012873.
- Wiedemann D, Schistek R, Gassner E, Antretter H. Mediastinal liposarcoma. J Card Surg. 2011; 26(2): 162-164. doi:10.1111/j.1540-8191.2010.01174.x.
- Grewal RG, Prager K, Austin JH, Rotterdam H. Long term survival in non-encapsulated primary liposarcoma of the mediastinum. Thorax. 1993; 48(12): 1276-1277. doi:10.1136/thx.48.12.1276.
- Chung C, Lu CC, Chang SC, Hsu WH, Perng RP. Mediastinal liposarcoma with local recurrence: A case report. Zhonghua Yi Xue Za Zhi Chin Med J Free China Ed. 1996; 57(1): 70-73.
- Erdös G, Tzanova I. Perioperative anaesthetic management of mediastinal mass in adults. Eur J Anaesthesiol. 2009; 26(8): 627-632. doi:10.1097/EJA.0b013e328324b7f8.
- Luckhaupt-Koch K. Mediastinal mass syndrome. Paediatr Anaesth. 2005; 15(5): 437-438. doi:10.1111/j.1460-9592.2005.01614.x.
- Li WWL, van Boven WJP, Annema JT, Eberl S, Klomp HM, et al. Management of large mediastinal masses: surgical and anesthesiological considerations. J Thorac Dis. 2016; 8(3): E175-E184. doi:10.21037/jtd.2016.02.55.
- Bacha EA, Chapelier AR, Macchiarini P, Fadel E, Dartevelle PG. Surgery for invasive primary mediastinal tumors. Ann Thorac Surg. 1998; 66(1): 234-239. doi:10.1016/s0003-4975(98)00350-6.