Introduction
Chronic Low Back Pain (CLBP) is a prevalent and debilitating
musculoskeletal problem that most people will experience at
some point in their lives [1]. The overall incidence of Low Back
Pain (LBP) is challenging to determine, as initial episodes are
notably prevalent by early adulthood, and there is a tendency
for symptoms to recur [1]. The etiology of LBP is multifactorial,
and weakness in core muscles is a significant factor leading
to less core support and trunk instability [1]. The abdominal
muscle group is an important part of the core muscles and
plays a pivotal role in stabilizing the lower spine and pelvis,
making them integral to overall posture [2]. A well-documented
connection exists between core muscle weakness and LBP, as
there is a recognized inverse relationship between abdominal
wall defects and abdominal muscle strength [3].
However, despite the recognized association between
core muscle weakness and LBP, there is a paucity of literature
exploring the link between ventral hernias and LBP. This
link remains unexplored, possibly due to the varied clinical
Annals of Surgical
Case Reports & Images
presentations of ventral hernias. Ventral hernias, or anterior
abdominal wall hernias, result from the protrusion of intraabdominal contents through congenital or acquired defects
in the transverse abdominis muscles [4]. These hernias often
develop due to repetitive stress on the abdominal wall. Obesity
significantly increases the risk of developing larger hernias and
elevates the likelihood of hernia recurrence [3]. Other factors,
such as ascites, coughing, vomiting, or pregnancy, can also
contribute to their development [5]. Ventral hernias can often
present with an asymptomatic mass or development of pain
from bowel strangulation and obstruction.
Currently, there are no standardized treatment guidelines
for asymptomatic ventral hernias, reflecting the complexity
of individualized patient scenarios. Surgeons may opt for
elective surgery or adopt conservative approaches like watchful
waiting, considering the patient’s risks, comorbidities, and life
expectancy [3]. In contrast, symptomatic hernias usually warrant
surgical care, with the majority requiring mesh placement. The
introduction of mesh repair has greatly reduced the recurrence
of ventral hernias to around 10-23% [6]. While more than 400,000 ventral hernia repair surgeries are performed annually
in the United States, ventral hernias are often easily ignored
due to the lack of imaging techniques and the unreliability of
clinical examination alone to make the diagnosis [7,8]. The
diagnosis of ventral hernias can often be overlooked without a
comprehensive physical examination. This case study explores
a 50-year-old male patient who experienced substantial relief
in LBP and promotion of back support following surgical ventral
hernia repair with mesh.
Case report
A 50-year-old male patient with past medical history of cervical fusion, cervicogenic headache, Gastroesophageal Reflux Disease (GERD), diverticulitis, and obesity presented to the clinic
with a 10- year history of LBP. Previously treated in the clinic
for his cervicogenic headache and neck pain, he described his
LBP as intermittent and dull, without radiating pain into his legs.
He denied any weakness or numbness in his bilateral lower extremities and denied acute bowel or bladder dysfunction. His
LBP worsened with back movement, particularly back twisting.
He typically could stand for only eight to ten minutes at a time.
He had tried several medications including Cymbalta, NSAIDs,
Tylenol, and had completed multiple physical therapy courses.
His physical examination revealed bilateral lumbar paraspinal tenderness at L4-L5, exacerbated by back extension and
lateral bending. Muscle strength, reflexes, and sensation to light
touch were normal in all extremities. An abdominal examination showed a bulge and a palpable mass that increased in size
with coughing and sit-ups. The bulge was reducible in a supine
position, and his Carnett’s sign was positive. His X-ray of lumbar
spine revealed mild facet joint arthropathy at L4-5 and L5-S1
and mild degenerative changes at the sacroiliac joints.
The patient was advised to undergo a diagnostic medial
branch nerve block for his lumbar facetogenic pain and referred
for a surgical consultation to evaluate a potential ventral hernia. At a five- month follow- up, the patient reported an 80%
improvement in LBP following Radiofrequency Ablation (RFA)
for his left- sided L4/5 and L5/S1 facet arthropathy/pain, after
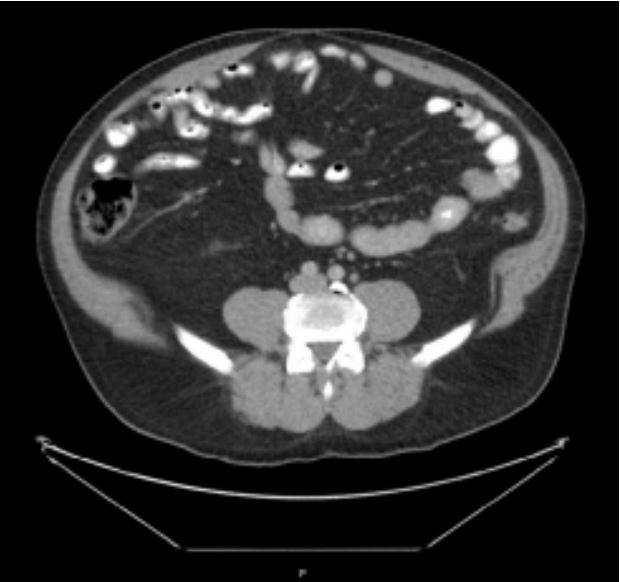
receiving two diagnostic medial branch nerve blocks. Additionally, a Computed Tomographic (CT) scan of his abdomen at an
outside facility confirmed a large abdominal wall defect, indicative of a ventral hernia (Figure 1). He subsequently completed
a ventral hernia repair surgery with a mesh. He endorsed additional relief of his LBP and enhanced back support, to which
he noted “feeling greater stability in my back” after his ventral
hernia repair. He was later followed in this clinic for continuity
of neck pain management.
Discussion
This case report draws attention to the multifactorial nature
of LBP and the less explored link between ventral hernias and
LBP. While ventral hernias can remain asymptomatic, some may
cause LBP due to their weakening impact on abdominal muscle
strength. Patients who present to the clinic with LBP are often
recommended to perform core strengthening, reconditioning,
and stabilization in the management of LBP [9]. However, in
this patient, the unaddressed ventral hernia would likely hinder
the effectiveness of physical therapy. This case illustrates that
surgical intervention may be necessary to fully address the root
causes of pain and enable effective rehabilitation.
Furthermore, this case underscores the indispensable role of
comprehensive physical examinations in the accurate diagnosis LBP. A thorough physical exam, coupled with a detailed
patient history, emerges as fundamental in guiding clinicians
toward making the correct diagnosis. However, the diagnostic
sensitivity of physical examinations for ventral hernias may be
significantly compromised among patients who have subtle
hernia presentations, those with a large body habitus, or
individuals with a complex surgical history [10]. Despite these
challenges, the current medical practice lacks a universally
accepted standard of care for diagnosing ventral hernias,
oscillating between physical examinations, imaging modalities
such as CT scans, ultrasound, MRI, and diagnostic laparoscopy
as potential options. With advancements in imaging technology,
CT scans are increasingly becoming the preferred method for
accurate diagnosis, offering superior precision over physical
examinations alone [10].
The patient’s clinical journey-from the initial presentation of
debilitating LBP through the diagnostic revelations of lumbar
facet arthropathy and a ventral hernia, to the symptomatic relief
following RFA for facetogenic LBP and the subsequent surgical
mesh repair of the ventral hernia-illustrates a compelling
narrative. This progression not only highlights the necessity of a
dual approach in addressing both the direct and indirect causes of
LBP but also underscores the evolving diagnostic and treatment
paradigms in the management of chronic LBP. By delving into
the complex relationship between structural anomalies like
ventral hernias and LBP, this case report contributes valuable
insights into broader LBP management strategies, advocating
for a more holistic, patient-centric approach that spans beyond
conventional treatments.
Conclusion
In conclusion, this case highlights the importance of
addressing core instability in CLBP patients and a reminder
to perform thorough physical examinations. This is especially
important prior to initiation of conservative treatments like
physical therapy as patients with abdominal wall defects will
likely be unable to take advantage of the benefits of physical
therapy. Significant ventral hernias are readily assessed on
physical exams; thus, clinicians should bear this condition
in mind when assessing for contributors to back pain in their patients. Further work is needed to clarify the role of ventral
hernia repair in improving chronic back pain. Preferably, future
studies should take the form of randomized control trials that
assess reporting outcomes of patients with chronic low back
pain and ventral hernias that had their hernia repaired or
elected to leave the defect unrepaired. Additionally, future
studies should focus on establishing the prevalence of hernias
in chronic low back pain patients and how severe these defects
tend to be.
References
- Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Practice & Research Clinical Rheumatology. 2010; 24(6): 769-781.
- Seo DK, Kim JS, Lee DY, Kwon OS, Lee SS, et al. The relationship of abdominal muscles balance and body balance. J Phys Ther Sci. 2013; 25(7): 765-7.
- Strigård K, Clay L, Stark B, Gunnarsson U, Falk P. Giant ventral hernia-relationship between abdominal wall muscle strength and hernia area. BMC Surgery. 2016; 16(1).
- Witt Michael, Brancato John C. Chapter 84 - Abdominal Hernias. Pediatric Emergency Medicine, edited by Jill M. Baren et al., WB. Saunders. 2008; 634-638.
- Good DW, Royds JE, Smith MJ, Neary PC, Eguare E. Umbilical Hernia Rupture with Evisceration of Omentum from Massive Ascites: A Case Report. Journal of Medical Case Reports. 2011; 5(1).
- Misiakos EP, Patapis P, Zavras N, Tzanetis P, Machairas A. Current trends in laparoscopic ventral hernia repair. JSLS: Journal of the Society of Laparoendoscopic Surgeons. 2015; 19(3).
- Harris HW, Primus F, Young C, et al. Preventing recurrence in clean and contaminated hernias using biologic versus synthetic mesh in ventral hernia repair. Annals of Surgery. 2021; 273(4): 648-655.
- Banker A, Gandhi J, Shinde P, Takalkar Y. Computed tomography for ventral hernia: Need for a standardised reporting format. Journal of Minimal Access Surgery. 2023; 19(1): 175.
- Barros G, McGrath L, Gelfenbeyn M. Sacroiliac Joint Dysfunction in Patients with Low Back Pain. Federal Practioner. 2019; 36(8): 370-375.
- Holihan JL, Karanjawala B, Ko A, et al. Use of Computed Tomography in Diagnosing Ventral Hernia Recurrence. JAMA.