Background
Behçet’s disease is an uncommon systemic inflammatory
vasculitis with an unidentified aetiology affecting both arteries
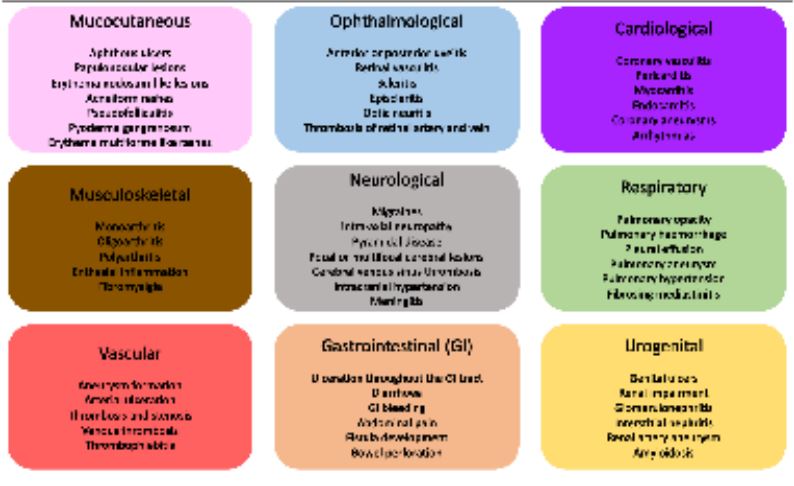
and veins [1]. BD can involve the mucocutaneous, musculoskeletal, vascular, ophthalmological, neurological, gastrointestinal,
cardio-respiratory, and urogenital systems with a relapsing-remitting course [1]. BD is a complex chronic condition which can
present with a varying number of symptoms and signs, mimicking other conditions and thus making it a challenging diagnosis
[1] (Figure 1). BD is most commonly seen in young males (20-40
years-old) with a high prevalence in the Middle East and Turkey
[1]. The International Study Group (ISG) criteria state that, for
a formal diagnosis there must be ‘presence of oral aphthosis
together with any two of; genital ulcers, ocular lesions, skin lesions and positive pathergy test’. More recently, the new International Criteria for Behcet’s (ICBD) includes the presence
of neurological and vascular manifestations [2]. Vascular manifestations such as arterial aneurysms, stenoses, occlusions, and
thromboses can affect up to 40% of patients with BD and are
more commonly seen in males [3]. Vascular manifestations of
Behcet’s present early on in disease progression and are associated with higher morbidity and long-term mortality. This case
highlights the importance of history taking and examination,
especially for an atypical vascular presentation.
Case presentation
A 25-year-old Moroccan gentleman presented to a London
district general hospital with a 4-week history of progressive left
leg pain, unable to weight-bear and requiring a stick for mobilisation. 48 hours prior to his admission his pain became unbearable even at rest with associated tingling sensation on his toes.
He was provided by his general practitioner paracetamol, ibuprofen, dihydrocodeine and oral morphine sulphate with no significant improvement. He denied any additional symptoms such
as cough, breathlessness, headaches, nausea, vomiting, chest or
abdominal pain and visual changes. Examination demonstrated
left proximal calf tenderness with associated localised swelling,
intermittent paraesthesia at L4/L5 dermatomes and preserved
pedal pulses with no other signs of compartment syndrome. A
neurovascular examination of the right leg was normal. Medical
history consisted of bilateral pulmonary embolisms (4-months
prior), right leg Deep Vein Thrombosis (DVT) (1-month prior)
and sport trauma with internal fixation to right tibia and fibula
(2014). He took regular paracetamol, morphine, amitriptyline
and therapeutic dose low molecular weight heparin (tinzaparin
sodium) injections, recently having switched from rivaroxaban
due to the development of DVT. He was allergic to sulfonamide
and aspirin. He had recently immigrated to the UK from Morocco with his wife and worked in a delivery warehouse. He was
a current smoker (7-pack years), with no alcohol or illicit drug
use history.
Initial Computed Tomographic Angiogram (CTA) of the lower
limbs demonstrated an irregular 3.7x1.5x3.1 cm (MLxAPxCC)
hypervascular lesion of the deep proximal left calf consistent
with a pseudoaneurysm with evidence of active extravasation.
He was transferred to a tertiary university hospital under the
vascular surgical team, where he underwent a left popliteal -
tibioperoneal trunk bypass with ipsilateral reversed great saphenous vein via a posterior approach, and ligation of the anterior tibial artery.
Investigations
Two days postoperatively, the patient reported sudden onset left calf and popliteal fossa pain with a cold foot and monophasic handheld doppler signal at the posterior tibial artery,
which was multiphasic the day before. He also developed a new
oxygen requirement with shortness of breath and tachycardia.
Given his past medical history he was investigated further with
a CTA of the lower limbs and a CT Pulmonary Angiogram (CTPA)
(See figures below). The former showed a large peripheral enhancing low attenuation collection surrounding the bypass graft
with an appropriately sited postoperative drain, the graft was
patent, with no evidence of extravasation. The latter showed
multiple thick-walled bilateral pulmonary artery aneurysms, the
largest of which measuring up to 2.2 cm, with no right heart
strain or evidence of infarction. Further questioning revealed a
history of recurrent painful mouth ulceration as well as genital
ulcers for the last 4-5 months. On re-assessment, examination
demonstrated pathergy at the cannula insertion site and findings consistent with anterior uveitis as well as oral and genital
aphthosis. Blood tests revealed the following:
A vasculitis screen was sent, this revealed a high ESR, WCC
and CRP in the context of recent major surgery. Immunoglobulins were all within normal limits and subsequent retroviral,
tuberculosis and syphilis screening were negative. Histology
results from the patient’s pseudoaneurysm reported findings
favouring an arteritis but were not discriminatory.
Table :
| Blood test |
Admission day |
2-days postoperatively |
Discharge day |
| Hb (g/L) |
125 |
114 |
116 |
| WCC (x10^9/L) |
10.34 |
14.92 |
20.75 |
| PLT (x10^9/L) |
396 |
446 |
794 |
| CRP (mg/L) |
160 |
375 |
6 |
| ESR (mm/hr) |
- |
100 |
- |
| Urea (mmol/L) |
3.7 |
4.6 |
6.1 |
| Creatinine (μmol/L) |
71 |
60 |
61 |
HB: Haemoglobin; WCC: White Cell Count; PLT: Platelets; CRP: C-
Reactive Protein; ESR: Erythrocyte Sedimentation Rate.
Discussion
BD is a complex chronic inflammatory condition with multiorgan involvement for which there is currently no formal diagnostic histopathological or laboratory confirmatory test [6].
Vascular manifestations of BD are commonly reported in central
and peripheral large arteries in the form of thromboses, aneurysms and pseudoaneurysms [1,3]. We present here a case of
young man with previous history bilateral pulmonary embolisms and lower extremity DVT, who presented to hospital with
limb ischaemia secondary to a popliteal pseudoaneurysm and
subsequently diagnosed with multiple high rupture risk pulmonary arterial aneurysms on a background of undiagnosed BD.
This is the first case in the UK to our knowledge that a popliteal pseudo-aneurysm and subsequently pulmonary aneurysms
lead to the diagnosis of BD. Similarly, a case report from India
described a 60-year-old man that had to undergo 4 vascular
surgeries for lower limb occlusion, thrombosis and aneurysms
prior to the diagnosis of Behcet’s disease [7].
Given the complexity of disease and varied presentation, patients with BD have poor prognosis if aneurysmal lesions are
identified, with pulmonary aneurysm being the most common
fatal complication in men [8]. A retrospective study from China
in 2019 showed that development of aneurysms happens in the
early stages of treatment naïve male BD patients, and new oral/
genital lesions or pathergy reactions can be independent risk
factors for aneurysm development [9]. Interestingly it has been
reported that BD patients with pulmonary artery aneurysms
usually present with haemoptysis, which was not observed in our patient [9,10].
Since 2018 the European League Against Rheumatism (EULAR) suggested that glucocorticoids and anti-TNF-α therapy
should be the mainstay of treatment in patients with aneurysmal lesions such as with our case. Immunosuppressive therapy
is believed to regress both thromboses and aneurysms [11,12].
In a retrospective study in Turkey, 70% of patients showed aneurysmal regression with aggressive treatment, nonetheless
20% of those recurred with a significant increase in the mortality rate [13]. It is important to note that TNF-α inhibitors can
be limited by intolerance, patient contraindications, inadequate
response or loss of efficacy and there is still increased need for
more evidence [11].
Acute arterial involvement must be managed as a medical emergency with intravenous methylprednisolone therapy,
appropriate rheumatology review and urgent initiation of immunosuppressive therapy [7,14]. BD patients with vascular
manifestations might also require surgical interventions such
as endovascular stenting, embolisation or open aneurysmectomy and/or bypass grafting. Management of a peripheral artery aneurysm is primarily determined by the clinical presentation, location of the aneurysm, risk of rupture and whether the
BD patient has active or controlled disease [14,15]. These patients remain a challenge for vascular surgeons as the vascular
inflammation increases the intra and post-operative risks and
complications. BD patients are also prone to recurrence of the
aneurysmal lesions requiring subsequent surgical interventions
[9]. Studies have shown the important contribution of medical
intervention with immunosuppressant medications either to
avoid surgical intervention or reduce the risk of postoperative
complications, thereby highlighting the need for appropriate
evaluation of medical and surgical intervention of aneurysmal
lesions in patients with BD [8,9,16]. A recent literature review
showed that endovascular treatment of vascular BD is increasingly preferred due to higher success rates and low recurrence.
Endovascular repair remains a safe alternative to traditional
open surgical intervention as it minimises endothelial injury
and reducing post-operative complications [17].
Conclusion
In conclusion, vascular manifestations have the leading
cause of death in BD patients and therefore early identification
and management is key. CTA remains a valuable imaging modality in the diagnostic work-up of BD [18]. Open and endovascular
surgical repair are available options for peripheral artery aneurysms with high recurrence rates thus highlighting the importance of early immunosuppressive therapy in BD.
Learning points
• When presenting with atypical vascular malformations
such as pseudo-aneurysms in young men, Behcet’s should
be considered in your differential diagnosis.
• Vascular thrombosis or occlusion can be a predictive factors for aneurysmal lesions in Behcet’s disease.
• Vascular manifestations of Behcet’s often present early,
and with concomitant vascular features
• Pulmonary aneurysms are life-threatening complications
of Behcet’s and clinicians should have a low-threshold for
investigating if any clinical suspicion.
Patient’s perspective
“Hello everyone,
Today I am here to tell you a short story about a medical
condition that I am currently going through and the meanings
and pain that I have experienced. First, it started with a sharp
pain in the right side of my chest, difficulty breathing and a high
temperature. I therefore, tried to call the ambulance and from
there the story became clear that there was something strange
going on in my body. For a few weeks I was also experiencing
some infections in my mouth, genitals, swelling of my legs and
difficulty sleeping. I decided to take this matter to my local hospital and after a lot of effort, patience and pain, I was told that I
have a chest infection. I was not sure where the problem came
from and after months of having lots of different tests I was diagnosed with multiple clots in my lungs and legs. Few weeks
ago, I started suffering from leg pain and I tried to return to the
hospital because the strong painkillers (morphine) that the GP
gave me did not help me. There I had a scan of my leg and suddenly I was transferred to another hospital for surgery. After the
surgery on my left leg, I had a scan of my chest which showed
aneurysms on my lungs. During that period in the new hospital
and by putting all of this together it was discovered what was
happening in my body as I was diagnosed with Bechet’s disease.
Here, I learned what is happening in my body thanks to the specialised medical team, so I learned about all the causes. I feel
better day by day and the condition will be monitored until the
end.
Well, it seems appropriate that my life story fits on one page.”
References
- Nair, Jagdish R, Robert J Moots. Behcet’s Disease. Clinical Medicine. Royal College of Physicians. 2017; 17: 71-77. doi:10.7861/clinmedicine.17-1-71.
- Kiafar, Mina, et al. Diagnosis of Behçet’S Disease: Clinical Characteristics, Diagnostic Criteria, And Differential Diagnoses. BMC Rheumatology. Springer Science and Business Media LLC. 2021; 5. doi:10.1186/s41927-020-00172-1.
- Demirtürk Orhan Saim, et al. Vascular Manifestations of Behçet’s Disease. Behcet’s Disease. 2017. https://doi.org/10.5772/intechopen.68765.
- Ambrose, Nicola L, Dorian O Haskard. Differential diagnosis and management of Behçet syndrome. Nature reviews. Rheumatology. 2013; 9(2): 79-89. doi:10.1038/nrrheum.2012.156
- Kreibich, Maximilian, et al. Aneurysms of the Pulmonary Artery. Circulation. 2015; 131(3): 310-316. https://doi.org/10.1161/circulationaha.114.012907
- Yazici, Hasan, et al. Behçet syndrome: A contemporary view. Nature reviews. Rheumatology. 2018; 14(2): 107-119. doi:10.1038/nrrheum.2017.208
- Jayachandran, Nambiar Veettil, et al. Multiple peripheral arterial and aortic aneurysms in Behcet’s syndrome: A case report. Clinical rheumatology. 2008; 27: 265-7. doi:10.1007/s10067-007-0713-z
- Schreiber, Benjamin E, et al. Resolution of Behçet’s syndrome associated pulmonary arterial aneurysms with infliximab. Seminars in arthritis and rheumatism. 2011; 41(3): 482-7. doi:10.1016/j.semarthrit.2011.02.006
- Zhou, Jiaxin, et al. The Clinical Features, Risk Factors, and Outcome of Aneurysmal Lesions in Behcet’S Disease. Journal of Immunology Research. Hindawi Limited. 2019; 2019: 1-8. doi:10.1155/2019/9198506.
- Voiriot, Guillaume, et al. Transcatheter embolotherapy of pulmonary artery aneurysms as emergency treatment of hemoptysis in Behcet patients: experience of a referral center and a review of the literature. Internal and emergency medicine. 2018; 13: 491-500. doi:10.1007/s11739-018-1817-y
- Hatemi, Gulen, et al. Update of the EULAR Recommendations for the Management of Behçet’S Syndrome. Annals of the Rheumatic Diseases BMJ. 2018. annrheumdis-2018-213225. doi:10.1136/annrheumdis-2018-213225.
- Alpsoy, Erkan. Behçet’s disease: A comprehensive review with a focus on epidemiology, etiology and clinical features, and management of mucocutaneous lesions. The Journal of dermatology. 2016; 43(6): 620-32. doi:10.1111/1346-8138.13381
- Seyahi, Emire et al. Pulmonary artery involvement and associated lung disease in Behçet disease: A series of 47 patients. Medicine. 2012; 91(1): 35-48. doi:10.1097/MD.0b013e318242ff37
- Hasanaghaei, Tarlaan, et al. Huge Femoral Artery Pseudoaneurysm in a Patient with Behçet’s Disease. The Egyptian Rheumatologist. 2017; 39: 267-270. https://doi.org/10.1016/j.ejr.2017.02.001
- Sato T, Matsumoto H, Kimura N, Okamura H, Adachi K, et al. Urgent Surgical Management of Deep Femoral Artery Aneurysm in a Patient with Pre-Vasculo-Behcet Status. Ann Vasc Dis. 2015; 8(2): 116-9. doi: 10.3400/avd.cr.15-00017.
- Kalko, Yusuf, et al. The surgical treatment of arterial aneurysms in Behçet disease: A report of 16 patients. Journal of vascular surgery. 2005; 42: 673-7. doi:10.1016/j.jvs.2005.05.057
- Ding ZY, Jin GN, Ai X, Li LY, Zheng P, et al. Endovascular Treatment of Behcet Disease With Recurrent Infrainguinal Arterial Pseudoaneurysms: A Case Report and Literature Review. Medicine (Baltimore). 2016; 95(19): e3545. doi: 10.1097/MD.0000000000003545.000
- Ceylan, Naim et al. Pulmonary and vascular manifestations of Behcet disease: imaging findings. AJR. American journal of roentgenology. 2010; 194(2): W158-64. doi:10.2214/AJR.09.276