Case presentation
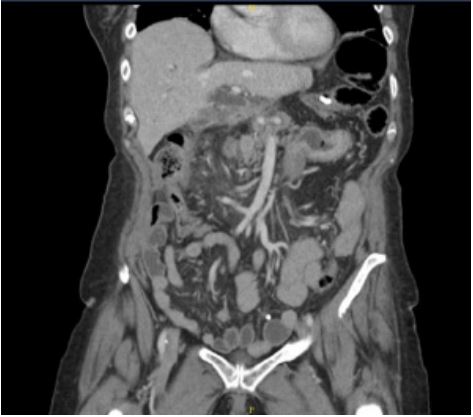
A 67-year-old female, with a history of a laparoscopic adjustable gastric band placed 20 years ago, was sent by her primary
doctor to the emergency department with worsening upper
and right lower quadrant abdominal pain. Outpatient CT scan
showed a dilated Common Bile Duct (CBD) with inflammation
of the ascending colon (Figure 1). She was admitted to the general medicine floor service with leukocytosis of 14,000 and liver
enzymes within the normal range. MRI of the abdomen showed
an adhesive band extending from the left upper quadrant to the
right lower quadrant, with an associated small bowel obstruction. Later that day, she had a 103F fever associated with an
increasing leukocytosis of 22,000/uL. A repeat CT scan showed
disconnected tubing tracking down to the right lower quadrant,
interval development of inflammation surrounding the band
and a small bowel obstruction with a transition point in the
right lower quadrant associated with free fluid in the pelvis and
right paracolic gutter (Figures 2 and 3). The surgery team was
consulted given the concern for small bowel obstruction associated with the patient’s prior bariatric surgery.
Intra-operatively, the small bowel was dilated and friable. In
examining the bowel, a decompressed terminal ileum was noted with significant dilation of the bowel proximal to fibrinous,
omental adhesions into the right lower quadrant. The center
of the inflammatory process contained a perforated, inflamed,
and injected appendix, which was removed. Adhesions of the
liver to the stomach were sharply divided. The transverse colon
was densely adherent to the area of the band and upon close
inspection, it was evident that the intra-abdominal band had
disconnected from the port tubing and eroded into the transverse colon. Furthermore, the band was eroded into the stomach. The band was carefully removed from both the transverse
colon and stomach and the enterotomies were closed primarily.
The gastrotomy was reinforced with an omental flap. The patient tolerated the procedure well, with no intraoperative complications. Pathology for the appendix resulted as acute transmural appendicitis with fibro purulent per appendicitis.
Given the intraoperative findings, the band seemed to be
chronically eroded into the stomach. The disconnection from
the tubing (it is unknown whether this was disconnected from a prior surgery or if it was the product of device failure) created
an exposed metal tip on the band side, which eroded into the
transverse colon. The band tubing was freely floating within the
abdomen when acutely, the patient developed an appendicitis.
The subsequent perforation caused the omentum and the associated tubing to migrate toward the right lower quadrant to
contain the perforation. With the band tubing draped toward
the right lower quadrant, this caused a small bowel obstruction
with a transition point in the right lower quadrant and compression of the CBD.
The patient’s post-operative course and recovery were uneventful and an upper-GI series on post-operative day 7 was
negative for leak. The patient was seen in clinic 3 months after
the surgery. She was tolerating a regular diet without issue and
reported regular bowel movements. She had no symptoms of
gastritis or reflux.
Discussion
Gastric band erosion into the stomach is a well-described
complication occurring in 1.6%-3% of cases [1]. Erosion into the
colon is less commonly observed, and the simultaneous erosion
of the gastric band apparatus into both the stomach and the
transverse colon is extremely uncommon. To our knowledge,
there are no original research studies that investigate the prevalence of gastric band erosion into both the stomach and the
colon simultaneously, and the pathology has been described in
only a few case reports [2-7].
There are two primary proposed etiologies for erosion at the
site of the gastric band: (1) elevated pressure caused by overfilling of the band or excessive food boluses and (2) rejection reaction against the silicon of the gastric band with circumferential
fibrosis [8]. It has further been previously proposed that repeated episodes of intra-abdominal infection may cause subacute
infection of gastric band and tubing, which, in the setting of friable colonic tissue, may predispose to erosion [2]. Furthermore,
it has been suggested that the most likely mechanism leading
to gastric band connecting tubing erosion is through bacterial
colonization of the tubing due to port infection [9]. Other proposed contributory factors for gastric band apparatus erosions
include hollow organ ischemia, NSAID use, vomiting, alcohol
consumption, and smoking history [10].
Our patient had an appropriately depressurized cuff at the
time of presentation and reported no findings or behaviors concerning for excessive food boluses, making a rejection reaction
the likely etiology. However, with regards to known modifying
factors that may predispose a patient to erosion, this patient
had no findings to suggest an ischemic process, nor did she have
a history of intraabdominal infection, signs of port-site seeding,
NSAID use, vomiting history, or alcohol use. The patient’s smoking history may have contributed to a basal inflammatory state
that put this patient at increased risk of erosion into both the
stomach and the transverse colon.
This patient’s acute presentation was likely secondary to her
appendicitis with progression to perforation, leading to omental displacement into the right lower quadrant, tracking the
free end of the band tubing with it, causing the observed small
bowel obstruction.
Conclusion
Erosion of adjustable gastric bands and the adjacent connecting tubes into the stomach or colon are rare, but relatively
well-documented complications of gastric banding. However, it
is exceedingly rare for a patient to present with simultaneous
erosion of the gastric band apparatus into two separate organs
as was the case in this patient’s erosion into the stomach and
transverse colon. It has previously been proposed that a history of intra-abdominal infection (namely port site infection or
recurrent diverticulitis), NSAID use, vomiting, alcohol use, and
smoking may predispose a patient to erosion. In this case, the
patient’s only known risk factor was her smoking history, which
may have contributed to a rejection reaction against the gastric band. We suggest counseling all patients with a history of
gastric band placement on smoking cessation and monitoring
all patients with risk factors for gastric band erosion carefully
for signs of erosion and perforation such as abdominal pain, inability to tolerate oral intake, signs of obstruction, and sepsis
as gastric band erosion is a pathology necessitating surgical or
endoscopic removal of the eroded foreign body and repair of
the eroded tissue.
Furthermore, clinicians should be aware of the possibility
of secondary complications in patients with a history of gastric
placement. As in this case, acute abdominal processes such as
perforated appendicitis can cause omental displacement and
the tracking of implanted hardware with it. Such hardware
mobilization should be considered as a potential etiology in patients with subsequent small bowel obstruction.
Financial disclosures: No disclosures to report.
Conflicts of interest: No conflicts to report.
References
- Schreiner MA, Fennerty MB. Endoscopy in the obese patient. Gastroenterol Clin North Am. 2010; 39(1): 87-97.
- Beh HN, Ongso YF. Simultaneous gastric and colonic erosions from gastric band and its tubing in the setting of recurrent intraabdominal infection. J Surg Case Rep. 2019; 2019(4): rjz102.
- Blouhos K, Boulas KA, Katsaouni SP, Salpigktidis, Mauroeidi B, et al. Connecting tube colonic erosion and gastrocolic fistula formation following late gastric band erosion. Clin Obes. 2013; 3(5): 158-61.
- Corvini M, Kang E, Weidner G, Lombert J. Laparoscopic Adjustable Gastric Band Erosion Into the Stomach and Colon. J Am Osteopath Assoc. 2018; 118(7): 479-81.
- Gonzalez LE, Kedar RP. Gastric and colonic erosion caused by laparoscopic gastric band: A case report. BJR Case Rep. 2017; 3(3): 20160135.
- Povoa AA, Soares C, Esteves J, Gandra A, Maciel R, et al. Simultaneous gastric and colic laparoscopic adjustable gastric band migration. Complication of bariatric surgery. Obes Surg. 2010; 20(6): 796-800.
- Tyrell R, Kukar M, Dring R, Gadaleta D. Simultaneous gastric and colonic erosion of gastric band. Am Surg. 2014; 80(1): E14-6.
- De Palma GD, Formato A, Pilone V, Rega M, Giuliano ME, et al. Endoscopic management of intragastric penetrated adjustable gastric band for morbid obesity. World J Gastroenterol. 2006; 12(25): 4098-100.
- Strahan A, Aseervatham R. Laparoscopic adjustable gastric band tubing erosion into large bowel. ANZ J Surg. 2017; 87(7-8): 631-2.
- Abu-Abeid S, Szold A. Laparoscopic management of Lap-Band erosion. Obes Surg. 2001; 11(1): 87-9.