Introduction
Residual Cyst (RC) is an odontogenic inflammatory pathology, described in the latest WHO Classification of Head and Neck
Tumours as a radicular cyst remaining in the jaws after the extraction of the affected tooth [1]. However, other odontogenic
and non-odontogenic maxillary entities, cystic or neoplastic,
can also mimic the radiological appearance of a residual cyst
[2].
The RCs represent up to 10% of all odontogenic cysts and are
mainly asymptomatic and slow-growing lesions [3]. The classical radiological appearance of RC is as a well-defined unilocular radiolucency with corticated margins [2], whose differential
diagnosis includes other odontogenic entities such as lateral
radicular cyst or odontogenic keratocyst. For these reason it is
very important to always perform a complete clinical history
and radiological examination before the surgical enucleation
[2]. In the last years, some RCs related to dental implants have
been described.
Material and methods
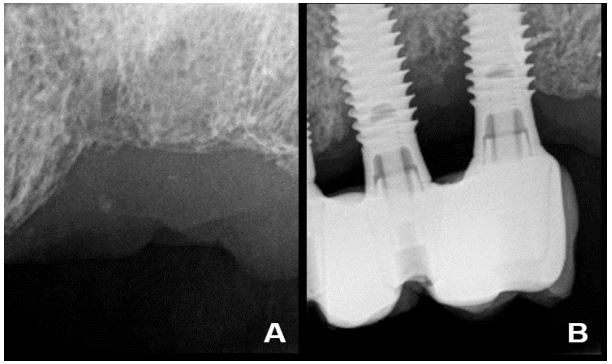
A 65-year-old heavy-smoker man with poor oral hygiene and
no medical history of interest, who referred pain in the upper
left maxilla, associated with three dental implants placed 11
years ago (positions 2.4, 2.5 and 2.6). The patient had a history
of a previous failed endodontic treatment in tooth 2.5 that left
an irregular radiolucent lesion following the extraction, which
was diagnosed as chronic periapical periodontitis (Figure 1A).
After 7 years of implant placement, he had an episode of periimplantitis and was treated with Er: Cr YSGG laser, after which he stopped maintenance therapy. At the present, 4 years later,
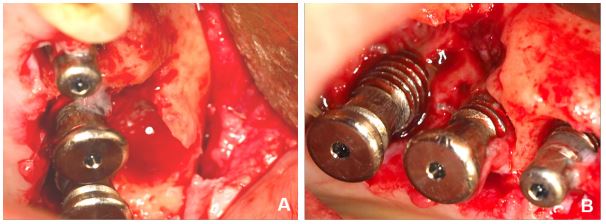
2.5 and 2.6 implants show great marginal bone loss and 2.5 implant has a 10 mm buccal probing depth (Figure 1B). During the
scheduled surgical treatment of peri-implantitis, a para-implant
membranaceus lesion was discovered adjacent to the implant
2.5, with persistence of the bony septum of separation between
the two bone defects (Figure 2).
Results
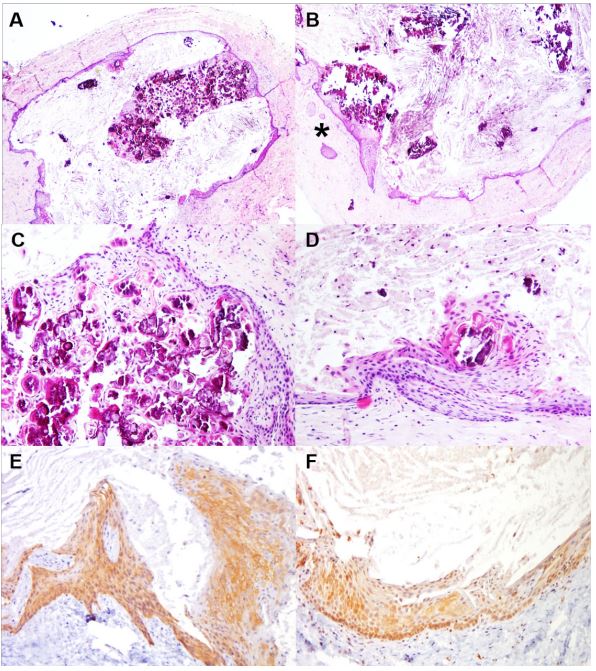
The histopathological analysis of the sample showed a welldefined cystic lesion with a dense fibrocelular connective tissue
wall without inflammation, with a few well-defined remnants of
odontogenic epithelium (Figure 3A-F). The cyst had a stratified
non-keratinized epithelial lining, mostly thin with thicker areas
with hyaline Rushton bodies. The immunohistochemical study
showed positive expression of cytokeratins 14 and 19, confirming the odontogenic origin of the epithelial lining. With all these
data, the final clinicopathological diagnosis was Para-implant
Residual Cyst.
One year later, the patient remains under maintenance therapy for dental implants, with no further alterations. There are
no signs of recurrence of the cystic lesion.
Table 1: Main clinical data of cases of para-implant residual cysts.
| Authors, year |
Sex/ Age |
Site |
Endodontic history |
Sign |
Symptom |
| Frantz et al. 2014 [6] |
F/59 |
Distal 1.2 |
Failed endodontic treatment
|
Purulent exudate in surgery
|
No |
|
Pistilli et al. 2020 [7]
|
F/28 |
Buccal 1.2 |
Dental fracture |
Swelling |
Discomfort |
|
Pistilli et al. 2020 [7]
|
M/25 |
Distal 3.7 |
Failed endodontic treatment
|
No |
Discomfort |
|
Pistilli et al. 2020 [7]
|
M/64 |
Distal 4.6 |
Unknown |
Swelling |
Discomfort |
| Current case |
M/65 |
Buccal 2.5 |
Failed endodontic treatment
|
Purulent exudate in surgery
|
Discomfort |
Discussion
The inflammatory RC is an odontogenic pathology that mainly appears in adult patients [4]. These lesions most frequently
develop in the posterior sector of the mandible [3,4]. Given
the absence of the initial inflammatory stimulus that triggered
the radicular cyst, RC usually presents with a dense fibrocelular
connective capsule and a milder inflammatory response [5]; in
some cases indistinguishable from development odontogenic
cysts [2,3]. The thin epithelial lining of RC is non-keratinized and
may show mucous metaplasia as well as different degrees of
superficial keratinization, which can make the final histopathological diagnosis difficult [2]. The presence of Rushton hyaline
bodies is also common in this pathology [1,2].
In this study, we present a special case of RC given its association with dental implants. This clinical scenario has motivated
us to review the current scientific literature, in order to identify other reported cases of RC associated with dental implants and
to discuss its main clinic pathological features.
To date, four cases of para-implant RC have been published
[6,7] (Table 1). The final five cases correspond to 2 females and
3 males, with a mean age of 48.2 years (range: 25-65). The lesions were located in the anterior and posterior sectors of the
jaws. The time of evolution from implant placement until the
diagnosis of the lesion ranged from 1 to 10 years. Para-implant
RCs were mainly discovered as an irregular radiolucency associated with loss of peri-implant supporting bone. Most patients
referred discomfort, and two of them also had a swelling at the
site of the lesion. After the surgical excision, all dental implants
maintained bone stability.
We believe that the pathogenesis of para-implant RC is similar to that of conventional RC. When the pulpal inflammatory
process reaches the periapical region, a chronic inflammatory
response in the periodontium leads to the activation and proliferation of the epithelial rest of Malassez, and the formation
of a cystic cavity that remains in the bone after tooth-extraction
[3]. The existence of a history of pulp pathology in all cases of
para-implant RC (root-canal treatment failure, tooth-fracture)
suggests that this factor is the starting point for these lesions,
and not the inflammatory process of peri-implantitis itself. Nevertheless, the existence of a peri-implant inflammatory disorder could reactivate it.
This para-implant pathology once again highlights the importance of making a good clinical history and radiological analysis in all patients. It is also necessary to perform an adequate
surgical curettage of the alveolus after toot-extraction, in order
to remove any material that may exist and always send it for
microscopic study. When facing a maxillary radiolucent lesion,
we must always proceed to its clinico-radio-histopathological
diagnosis and treatment, prior to the dental implant placement.
Same way, it should not be forgotten that “not all peri-implant
inflammatory lesions correspond to peri-implantitis” [8]. Finally, although RC is an initially benign odontogenic disorder, cases
of malignant transformation have also been reported in this
pathology [9], which emphasize the importance of its correct
diagnosis, treatment and control.
Conclusion
In summary, para-implant RC is an uncommon pathology
but whose appearance justifies performing a complete clinical history and radiological examination in all patients undergoing dental implant therapy, and those who had a previous
odontogenic inflammatory pathology. These patients should be
actively monitored for early diagnosis and treatment of periimplant disorders, including odontogenic cysts.
The patient previously signed an informed consent. This
study follows the principles of the Declaration of Helsinki on
Ethical Principles for Medical Research Involving Human Subjects, and has been approved by the UPV/EHU Research Ethics
Committee (CEISH: M10/2016/057).
Acknowledgments: This research did not receive any specific grant from funding agencies in the public, commercial or
not-for-profit sectors.
References
- Speight P, Tekkeşin MS. Odontogenic cysts of inflammatory origin. In: El-Naggar A, Chan J, Grandis J, Takata T, Slootweg P. WHO classification of head and neck tumours. Lyon: IARC Press. 2018; p232-233.
- Shear M, Speight PM. Cysts of the oral and maxillofacial regions. 4rd ed. Oxford: John Wiley & Sons. 2007.
- Main DMG. Epithelial jaw cysts: A clinic pathological reappraisal. Br J Oral Surg. 1980; 8(2): 114-125. https://doi.org/10.1016/S0007-117X(70)80002-6
- Titinchi F, Morkel J. Residual cyst of the jaws: A clinico-pathologic study of this seemingly inconspicuous lesion. Plos one. 2020; 15(12): e0244250. https://doi.org/ 10.1371/journal.pone.0244250
- Harris M, Toller P. The pathogenesis of dental cysts. Br Med Bull. 1975; 31(2): 159-163. https://doi.org/10.1093/oxfordjournals.bmb.a071273
- Frantz BJ, Caton JG, Bonacci FJ, Geminiani A, Arseneau R, et al. Peri‐Implant Cystic Lesion with Unusual Cellular Changes: A Case Report. Clin Adv Periodont. 2014; 4(4): 240-245. https://doi.org/10.1371/journal.pone.0244250
- Pistilli R, Canullo L, Menini M, Pistilli V, Rossi-Fedele G, et al. Retrograde peri-implantitis associated with residual cysts: 3 Case reports. JADA. 2020; 151(12): 956-961. https://doi.org/10.1016/j.adaj.2020.07.016
- Sotorra‐Figuerola D, Lafuente‐Ibáñez de Mendoza I, Parra‐Pérez C, Aguirre‐Urizar JM. Histopathological analysis of biopsies of “peri‐implant inflammatory lesions.” Everything is not what it seems. Clin Implant Dent Rel Res. 2020; 22(3): 366-372. https://doi.org/10.1111/cid.12905
- Van der Waal I, Rauhamaa R, Van der Kwast WAM, Snow GB. Squamous cell carcinoma arising in the lining of odontogenic cysts: report of 5 cases. Int J Oral Surg. 1985; 14(2): 146-152. https://doi.org/10.1016/s0300-9785(85)80086-7.