Introduction
The prevalence of diabetic foot OM has been estimated at
23.5% in outpatient settings and 66% in hospitalized patients
[1]. Additionally, it globally affects the forefoot more frequently
(90%), followed by the midfoot (5%) and the hindfoot (5%) [2].
The therapeutic objectives in this condition are infection reso�lution and restoration of limb functionality, this objective is
reached mainly through surgery, long-term systemic antibiotics
and physical therapy.
Surgical treatment involves debridement of devitalized tis�sues, irrigation, and bone resection with infection-free margins
[2], the intervention could also include management of dead
space and wound, bone stabilization, and bone grafting in the
case of large bone defects. This procedure may impact foot me�chanics, often necessitating amputations at various functional
levels of the limb [3]. The risk of amputation above the ankle is
significantly higher when OM is present in the hindfoot (50%)
compared to the midfoot (18.5%) and the forefoot (0.33%) [2].
Often, after surgery patients have to go through a long reha�bilitation process because of the change in the foot structure.
Some alternative techniques have been described, but the most
used one seems to be the amputation. The objective of this ar�ticle is to describe the treatment with bone curettage and filling
with antibiotic-loaded cement in a diabetic patient with chronic
OM of the midfoot and its mid-term clinical outcomes.
Case presentation
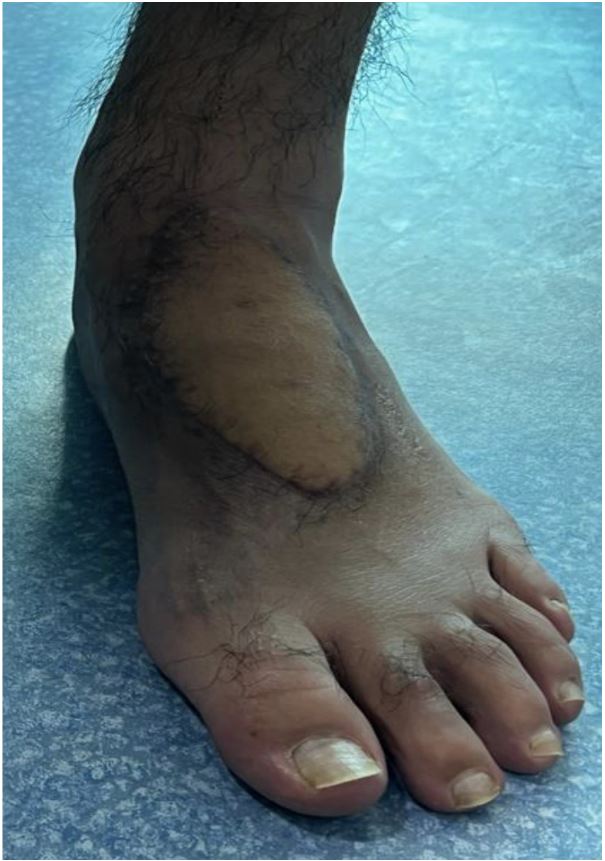
A 32-year-old male patient, with a history of Type I Diabetes
Mellitus, bilateral pes planus valgus, and arterial hypertension,
arrives at the emergency department due to month and a half
evolving condition consisting of a wound on the left foot caused
by a burn with boiling water, initially managed with dressings
and oral antibiotic treatment. Increased inflammation, pain, and functional impairment are noted in the left foot. Labora�tory tests reveal elevated inflammatory markers and a Magnetic
Resonance Imaging shows findings consistent with OM of the
base of the first metatarsal and the medial margin of the first
cuneiform of the left foot, along with a pericapsular laminar col�lection.
Patient is hospitalized for intravenous antibiotic manage�ment, surgical cleansing, and the insertion of a cement spacer
impregnated with antibiotics. During the first surgical cleansing,
devitalized tissue is excised, and pockets discharging purulent
fluid are observed. Cement impregnated with Ceftazidime and
Vancomycin is placed, and an aspirating Vacuum Assisted Clo�sure is installed. Two more surgical cleansings are performed
in the following days, without any new relevant findings. The
patient receives a total of 14 days of intravenous antibiotic
treatment and undergoes microsurgical Free Flap reconstruc�tion. Due to a favorable evolution, is discharged with intrave�nous antibiotic management to complete 4 weeks and wound
care. Follow-up appointments were conducted at 2,3,4,6, and
12 months, in which the patient exhibited no signs of infection
recurrence, without clinical or radiological deformity, and re�ported pain free-motion as well as other favorable outcomes
through self-reported questionnaires.
Discussion
Treatment of OM is perhaps the most controversial area re�garding the management of complications in diabetic foot care.
Physicians often have to make decisions about its management
with inadequate data, largely due to the scarcity of evidence on
the subject, resulting in heterogeneity and uncertainty in prac�tice. The usual approach for a condition like this would typically
involve amputation through the Lisfranc joint [3].
It has been described that the use of antibiotic-loaded ce�ment combined with systemic antibiotic therapy may reduce
the number of amputations, preserving greater stability and
biomechanics of the foot [4]. Regarding the management of
OM in diabetic feet, the use of antibiotic-loaded cement could
be a functional mid-term alternative. It is known that an ideal
surgical plan should also prioritize the preservation of weight�bearing capacity whenever feasible. In accordance with the
outcomes delineated in this article, it appears reasonable to
propose the integration of less invasive methodologies in the management of this pathology. Such approaches more ef�fectively preserve the foot’s anatomy, potentially facilitating
enhanced recovery and functionality. Currently, there are no
large-scale studies that objectively compare both alternatives
in terms of functional outcomes, but there are reported case
series with favorable results for the presented management [5].
Conclusion
Antibiotic cement is a tool with favorable outcomes in the
management of OM in diabetic feet, and its proper use could
reduce the need for amputation in certain situations. However,
the current evidence available does not allow for general rec�ommendations for all patients with these conditions. Clinical
judgment must be combined with a thorough understanding of
the specific clinical situation of each patient. Further research
would be helpful to demonstrate that local antibiotic treatment
with cement could be equally effective as amputation without
the morbid and functional implications that the latter option
entails.
References
- Giurato L, Izzo V, Meloni M, Uccioli L. Osteomyelitis in diabetic
foot: A comprehensive overview. World J Diabetes. 2017; 8(4):
135-142.
- Chan CSY, Malhotra R, Nather A. Osteomyelitis in the diabet�ic foot. Diabetic Foot & Ankle. 2014; 5(1). doi: 10.3402/dfa.
v5.24445.
- Nather A, Wong KL. Distal amputations for the diabetic foot. Dia�betic Foot & Ankle. 2013; 4(1). doi: 10.3402/dfa.v4i0.21288.
- Park J, Seok H, Woo I, et al. The Fate of Antibiotic Impregnated
Cement Space in Treatment for Forefoot Osteomyelitis. J Clin
Med. 2022; 11(7): 1976. doi: 10.3390/jcm11071976.
- Melamed EA, Peled E. Antibiotic impregnated cement spacer for
salvage of diabetic osteomyelitis. Foot Ankle Int. 2012; 33(3):
213-219. doi: 10.3113/FAI.2012.0213.