Introduction
Non-alcoholic fatty liver disease has a high prevalence now
in both developed or developing countries, and occurs frequently in obese patients. NAFLD contains simple steatosis, steatohepatitis, cirrhosis and can even develop into hepatocellular
carcinoma and liver failure. With the increase of NAFLD, hepatic
steatosis can be found in some non-obese patients with liver
injury through liver biopsy. Given the invasion of liver biopsy,
the relationship between NAFLD and non-obese patients can be
easily neglected, especially accompanied with drug and autoimmune factors. Here, we report such a case and hope to help
clinicians to diagnose these sorts of subjects.
Case presentation
A 45-year-old male Chinese complained to have the elevated
alanine aminotransferase (ALT) and aspartate aminotransferase
(AST) for four months. ALT [133 IU/L, normal value (nv): 9-50]
and AST (58 IU/L, nv: 15-40) were accidently found to be abnormal four months ago, while he was admitted to receive surgery
due to right tibial fracture. As he experienced severe trauma and
took some non-steroidal anti-inflammatory drugs amid the inhospitalization, he was discharged and operated the “Wait and
Watch” strategy on the issue of abnormal aminotransferases.
During the follow-up, he did not take any medications, however,
repeated liver function tests (LFTs) showed that ALT fluctuated
between 100 and 200 U/L, and AST fluctuated between 50 and
100 U/L. The patient did not have any clinical manifestations,
such as fatigue, loss of appetite, fever, jaundice and abdominal
pain. Besides, he did not have the history of alcohol consumption, viral hepatitis, hypertension, or diabetes mellitus. Physical examination revealed the normal blood pressure (109/61
mmHg), normal heart rate (70beats/min), along with normal
body mass index (BMI) of 21.5 kg/m2
. Unremarkable signs were
found. A series of laboratory tests were performed, and the results were as below: normal hemoglobin and leukocyte count
with a decreased platelet count (85×109
/L, nv: 100-300×109
),
normal bilirubin (0.48 mg/dl, nv: 0.29-1.64) and elevated ALT
(136 IU/L) and AST (65 IU/L), normal alkaline phosphatase
(ALP, 67 IU/L, nv: 45-125) and mildly increased gamma glutamyl transpeptidase (γGT, 84 IU/L, nv: 10-60); normal serum triglyceride (118.59 mg/dl, nv: 25.67-161.96), cholesterol (429.44
mg/dl, nv 247.93-504.71), and high density lipoprotein (39.33
mg/dl, nv: >34.70); normal fasting glucose (81.45 mg/dl, nv:
70.28-106.32); normal serum ceruloplasmin (339 mg/L, nv:150-
600), and normal coagulation tests. In addition to those listed
before, hepatitis B surface antigen and hepatitis C antibody
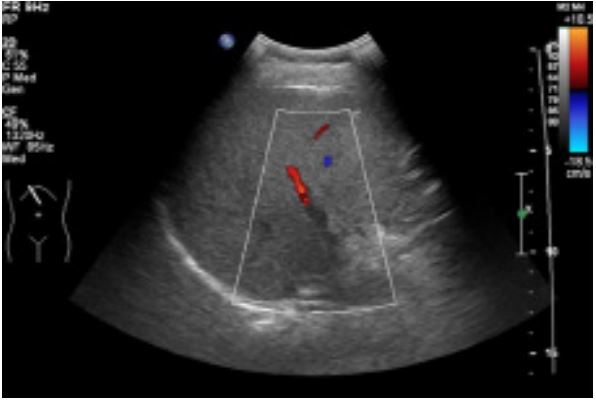
were negative, but antinuclear antibody and antimitochondrial antibody-M2 are suspicious. Diffused echo enhancement was
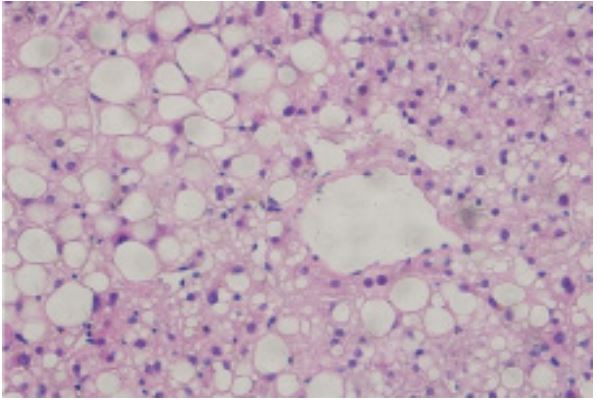
found in the liver under abdominal ultrasound sonography (Figure 1). Afterwards, liver biopsy was performed and intriguingly,
it showed that 80% hepatocytes were implicated with macrovesicular-dominant steatosis, along with scattered ballooning degeneration and infiltration with lymphocytes, monocytes and
a few of eosinophils (F4G2S1) (Figure 2). Herein, non-alcoholic
steatohepatitis (NASH) was confirmed, and patient received
lifestyle intervention and vitamin E. His aminotransferases restored to normal after three months.
Discussion
Non-alcoholic Fatty Liver Disease (NAFLD) occupied the highest rank among all kinds of chronic liver diseases, with a global
prevalence of 25.24% [1]. NAFLD is categorized into two forms
- Non-alcoholic Fatty Liver (NAFL) and NASH, the latter of which
is presented with marked inflammation and is more probably
progressed to fibrosis, and even cirrhosis [2]. Insulin resistance
is the key pathophysiological component of NAFLD, usually accompanied with obesity, type 2 diabetes mellitus, hyperlipidemia and hypertension.
Obese or overweight patients with the abnormal LFT could
strongly suggest the probability of NASH to physicians. However,
8-19% patients with NAFLD fall into the non-obese populations
[3]. Anyway, insulin resistance is still the core part of non-obese
NAFLD/NASH, but it revealed certain special clinical features.
BMI is most widely used to assess whether an individual is obese,
overweight or not, but it cannot reflect the visceral fat accurately, especially the distribution of fat in the abdominal cavity
[4]. Comparing with obese NAFLD, non-obese NAFLD may have
more visceral fat, which is the key to the disease progression [5].
Because of the risk of NAFLD progression to fibrosis and cirrhosis, it is meaningful to confirm the diagnosis of NAFLD in
non-obese populations with non-invasive measures. Although
several biochemical models have been developed to predict
the presence of NAFLD, however, with a high sensitivity of 85%
[6], ultrasound sonography is still most widely used to screen
out NAFLD. For LFTs, besides ALT and AST, γGT is most common
found to be abnormal for it elevates in more than 70% NAFLDs
[7], which could be a clue of diagnosing NAFLDs.
Another lesson drawn from this case is the role of antibody
in NAFLD. Although antibodies, such as ANA and AMA-M2, are
the important indicator of autoimmune liver diseases, however, they could be found to be false positive in some NAFLDs. A
Japanese study reported that 48% of NASH cases were positive
for ANA or AMA and were presented with the similar histological signs of AIH and PBC, especially in elder obese women [8].
Furthermore, another retrospective study showed that 34% of
NASH had positive ANA and 6% were ASMA positive [9]. Therefore, for patients with NASH clinical features and positive antibody, liver biopsy would be considered, and differentiated diagnosing should be carefully undertaken.
Above all, NASH should be considered its probability among
liver injury patients with non-obese somatype. False positivity
of antibodies could be observed in NAFLD, which might confuse
the confirmation of diagnosis.
Declarations
Acknowledgements: Not applicable.
Funding: No funding was received.
Availability of data and materials: Datasets used and/or
analyzed during the present study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate: Not applicable.
Patient consent for publication: The patient provided permission to publish the case details and images.
Competing interests: The authors declare that they have no
competing interests.
References
- Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64: 73-84.
- Golabi P, Stepanova M, Pham HT, et al. Non-Alcoholic Steatofibrosis (NASF) can independently predict mortality in patients with Non-Alcoholic Fatty Liver Disease (NAFLD). BMJ Open Gastroenterol. 2018; 5: e000198.
- Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol 2017; 67: 862-873.
- Katsuki A, Sumida Y, Urakawa H, et al. Increased visceral fat and serum levels of triglyceride are associated with insulin resistance in Japanese metabolically obese, normal weight subjects with normal glucose tolerance. Diabetes Care. 2003; 26: 2341-2344.
- Feng RN, Du SS, Wang C, et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World J Gastroenterol. 2014; 20: 17932-17940.
- Hernaez R, Lazo M, Bonekamp S, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver : A meta-analysis. Hepatology. 2011; 54: 1082-1090.
- Armstrong MJ, Houlihan DD, Bentham L, et al. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol. 2012; 56: 234-240.
- Tsuneyama K, Baba H, Kikuchi K, et al. Autoimmune features in metabolic liver disease - a single - center experience and review of the literature. Clinic Rev Allerg Immunol. 2013; 45: 143-148.
- Cotler S, Kanji K, Keshavarzian A, et al. Prevalence and significance of autoantibodies in patients with non-alcoholic steatohepatitis. J Clin Gastroenterol. 2004; 38: 801-804