Case presentation
An 88-year-old female patient presented to the emergency
department with a 12-hour history of mildly painful right inguinal bulge. She admitted to intermittent nausea but denied vomiting or fever. Physical examination revealed slightly distended
abdomen with normal bowel sounds, and a non-reducible right
groin bulge measuring 5x5 cm associated with skin erythema.
Laboratory test findings indicated leukocytosis (11,350/
mm³). Abdominal ultrasonography showed a complicated right
inguinal hernia with a 46x30 mm sac. Within the sac, a non-peristaltic tubular structure measuring 9.1 mm in diameter was observed, suggestive of the appendix. Adjacent peri-appendiceal
fat stranding and the presence of free fluid were noted (Figure
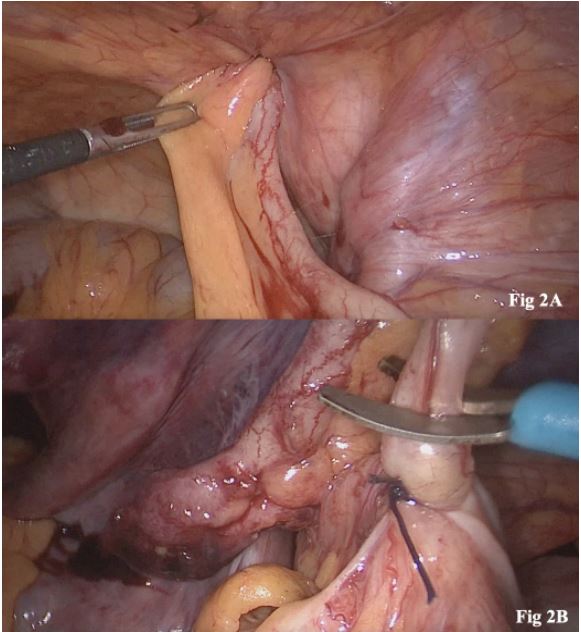
1). Based on the clinical findings and diagnostic imaging, the patient was admitted for a laparoscopic exploration that revealed
an incarcerated right femoral hernia (Figure 2A). The first step
was to reduce the hernia content through blunt maneuvers and
gentile traction, and a phlegmonous appendix with no signs of
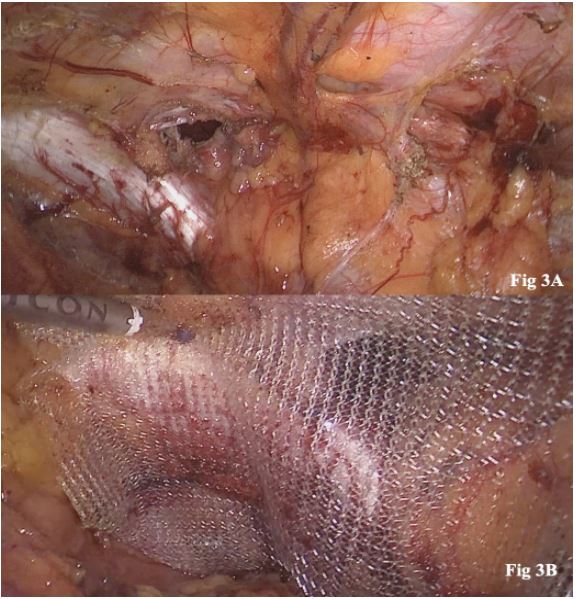
perforation was observed. Subsequently, a laparoscopic appendectomy was performed (Figure 2B), and the abdominal cavity
and the hernia sac were thoroughly irrigated with saline solution. Finally, a transabdominal preperitoneal (TAPP) hernia repair with a polypropylene mesh was done (Figure 3A-B). The
patient had an uneventful recovery and was discharged on the
second postoperative day with oral antibiotic treatment for 7
days. No complications were recorded at 30-day follow-up and
histopathologic results revealed acute appendicitis.
Discussion
The eponymous De Garengeot hernia, characterized by the
presence of the appendix within a femoral hernia, was first
described by the French surgeon René-Jacques Croissant De
Garengeot in 1731. It’s a rare presentation, with an estimated
incidence ranging from 0.15% to 5%. These are predominantly
encountered in elderly, multiparous individuals, with approximately 40% of the cases presenting as obstructions or strangulations scenarios [1]. Groin bulge or groin pain are the most
common presenting symptoms. Skin erythema is reported in
33.3% of cases [2]. An overall lack of abdominal symptoms, especially in cases where the appendix was perforated, can likely be explained by the constrictive and narrow diameter of the
femoral canal, which may prevent the spread of inflammation
into the abdominal cavity [2].
Diagnosis is frequently established during surgery (89.5% of
cases); however, when diagnosed preoperatively, the majority
are identified through CT scans with a sensitivity of 61%. The
small percentage of preoperative images may be due to the acute
clinical presentation of suspected inguinal hernia incarceration,
which often makes radiological investigations unnecessary.
The initial management involves resuscitation and subsequent surgical exploration. Surgical objectives include reducing
the hernia sac, performing the appendectomy, and repair the
femoral defect. There is no consensus regarding the optimal
surgical approach or the use of synthetic mesh for the hernia
repair [2]. There is considerable variation in the choice of surgical techniques for complicated hernias. The most common
approach has traditionally been open surgery with an isolated
groin incision. In some cases, this may be accompanied by a laparotomy when encountering difficulties in accessing the base
of the appendix or assessing the cecum. On the other hand,
laparoscopic surgery is increasingly becoming a viable option
for general surgeons in abdominal wall surgery. The advantage
of this approach lies in its capacity to assess the intraperitoneal
cavity, thereby aiding in bowel evaluation, allowing the ability
to perform the hernia reduction procedure under direct vision
and, allowing for the preferred laparoscopic hernia repair, as
well as potential bowel resection if required. When there is a
low clinical suspicion of a contaminated field, a femoral hernia
repair with the use of a synthetic mesh should be the preferred
option since it has been associated with a reduced hernia recurrence rate. In the presence of a perforation or gross contamination, a suture repair is commonly chosen to reduce the risk of
a mesh-bound infection, although, new investigations suggest
the feasibility of mesh repair in contaminated fields [3]. Individual surgeons probably benefit from applying their standard
techniques rather than choosing a specific method.
In conclusion, De Garengeot hernias present a unique diagnostic challenge. They are more common in elderly women and
had higher risk of obstruction and strangulation. Laparoscopic
approach is a suitable alternative for the management of this
rare entity since it allows to assess the intraperitoneal cavity
and to perform an appendectomy and mesh repair if it was decided, maintaining the benefits of the minimal invasive surgery.
Conflicts of interest and source of funding: Nicholas S Murdoch Duncan, María A. Casas and Emmanuel E. Sadava have no
conflict of interest, financial ties or funding/support to disclose.
Ethical approval: The Institutional Review Board (IRB) approved this work.
References
- Kalles V, Mekras A, Mekras D, Papapanagiotou I, Al-Harethee W,
et al. De Garengeot’s hernia: A comprehensive review. Hernia.
2013; 17: 177-82.
- Olivero AA, Casas MA, Angeramo CA, Schlottmann F, Sadava
EE. Outcomes after laparoscopic transabdominal preperitoneal (TAPP) hernia repair in the emergency: A matched case-control
study. Int J of Abdominal Wall and Hernia Surg. 2022; 5: 77-82.
- Casas MA, Dreifuss NH, Schlottmann F, Sadava EE. Safety and
Long-Term Outcomes after Hernia Repairs with Synthetic Mesh
in Contaminated Fields. J Gastrointest Surg. 2020; 24: 2849-2851.