Introduction
Atraumatic Splenic Rupture (ASR) is a rare pathological entity relative to traumatic cases, being referred to as a spontaneous rupture in the presence of a histologically proven normal
spleen, conversely nomenclature stipulates it is referred to as
a pathological rupture in diseased spleens [1]. ASR carries with
it a risk of mortality which has been reported to be as high as
12.2% [2], given the life-threatening potential a prompt diagnosis and subsequent management is critical. However, the aetiology of ASR is wide ranging and often and the clinical diagnosis
can be obscured by signs and symptoms being attributed to the
underlying disease process, thus requiring a high index of clinical suspicion.
Case presentation
A 41 year old female with no past medical history of note
presented to the emergency department with a 3 day history
of coryzal symptoms, a productive cough of yellow sputum, exertional shortness of breath, left sided pleuritic chest pain, myalgia and confusion. She was a previous cigarette smoker with
a 9 pack year history and was currently vaping. Initial observations on admittance to hospital revealed an Early Warning Score
(EWS) of 1 for a blood pressure of 106/64 mmHg, clinical examination was unremarkable beyond scanty left basal crepitations
on auscultation, biochemical anomalies were a c-reactive protein of 83, platelet count 80x109
/L, prothrombin time 11.5 seconds and a lymphocyte count 0.36x109
/L with a normal overall white cell count. A chest x-ray revealed left lower zone patchy
infiltrates and a respiratory viral screen returned positive for
influenza B virus. She was commenced on intravenous antibiotics and oral oseltamivir for viral pneumonia with suspected
secondary bacterial infection, being transferred to a respiratory
ward. On day 2 of her admission she complained of worsening
left sided chest/hypochondriac pain and continued to be hypotensive, presumed to be secondary to the underlying infection,
before rapidly deteriorating later in the evening with an EWS
of 10. A venous blood gas revealed a metabolic acidosis with
a lactate of 5.6 mmol/L and a Haemoglobin (Hb) 7.8 g/dl. She
was treated initially for septic shock before a repeat blood gas
shortly after boluses of intravenous fluid showed a falling Hb
to 4.4 g/dl, confirmed on laboratory results. The major haemorrhage protocol was declared with administration of blood
products to also correct clotting before transfer to radiology for
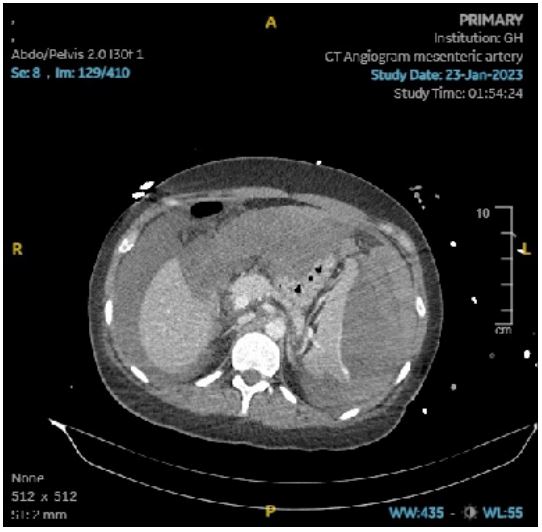
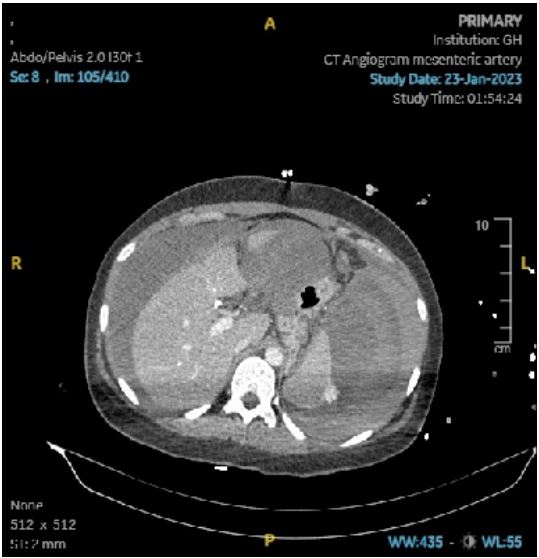
an urgent CT chest, abdomen and pelvis with a mesenteric angiogram. Imaging findings revealed a subcapsular splenic haematoma, with extensive intraperitoneal extension and active
contrast extravasation consistent with ongoing haemorrhage
confirming ASR with an American Association for the Surgery of
Trauma (AAST) grade 4 splenic injury. This was alongside scattered patchy consolidative changes throughout the lungs, with
atypical appearances, sparing the dependant areas being predominantly limited to the peri-hilar and anterior segments of
the upper lobes as well as the right middle lobe and left lingula.
The patient underwent an emergency open splenectomy later
that evening. She made an uneventful recovery and was discharged home at day 7. Macroscopically the specimen was of
normal appearances apart from the obvious haemarrhage. Microscopically the specimen retained architecture of the white
pulp with normal immunohistochemistry, there was some expansion of the red pulp indicating a degree of mild congestion
but no specific cause of the splenic rupture was identified.
Table 1: Examples of aetiology.
| Aetiology |
Examples |
| Neoplatic |
Hodgkin’s symphoma and
primary/secondary
neoplas-
tic disorders
such as angiosarcoma and
lung cancer
|
| Infectious |
Viral, bacterial, fungal or
protozoal in nature such
as
malaria
|
| Inflammatory |
Pancreatitis, systemic lupus
erythematosus
|
| Treatment related |
Haemodialysis, oral
anticoagulants
|
| Mechanical disorders |
Pregnancy, congestive
splenomegaly secondary to
liver
cirrhosis and portal
hypertension
|
Discussion
The management of ASR can be broadly divided into surgical
with either a total splenectomy or organ preserving surgery and
non-surgical with arterial embolization or conservative “watchful waiting”. Whilst there remains no generalised consensus,
the decision is influenced by a number of factors including, but
not limited to, the degree of haemodynamic instability and ultimately the clinical condition of the patient, grade of splenic
injury, availability of specialist interventional radiology services
for arterial embolization and the suspected cause, with malignant causes favouring total splenectomy [3]. In a large systematic review of ASR Renzulli et al found that of 774 patients,
85.3% underwent surgery within 24 hours and of the remainder
managed non-surgically, 17% eventually underwent secondary splenectomy due to rebleeding and haemodynamic compromise [2]. However the benefits of non-surgical management
must not be disregarded due to the spleens fundamental role
in immunity and conferring protection against encapsulated
organisms [4]. The underlying aetiological association of ASR
is expansive and can be broadly categorised into distinct subgroups [2,5].
Of the above sub-groups Renzulli et al. found that malignant
haematological, viral infectious and inflammatory disorders accounted for 42.1% of the 845 patients [2]. In a systematic review of ASR in 613 patients, Aubrey-Bassler et al found that the
most common associated pathological processes were infectious in nature [6]. ASR may present with an array of clinical
symptoms and signs obfuscating an accurate and time critical
diagnosis. This is further compounded by the wide variety of
aetiological conditions which may contribute to it. Given the associated high mortality, and can be attributed to any number
of the associated aetiological conditions. Patients may present
with abdominal pain, not solely in left upper quadrant as commonly depicted in textbooks as a result of hemoperitoneum
thus imitating commoner causes of an acute abdomen. They
may also present in the absence of any pain and instead with
vague symptoms of shoulder tip pain referred to as Kehr’s sign,
chest pain, nausea and vomiting as well as weakness [7].
Conclusion
To summarise we have outlined the first documented case of
a spontaneous splenic rupture associated with Influenza B virus
in English literature. Although the majority of patients with ASR
will undergo an emergency splenectomy, non-surgical management such as splenic artery embolization should be considered
in clinically appropriate cases to preserve splenic function and
thus avoid the need for vaccinations and lifelong antibiotic therapy. The associated pathological entities of ASR are vast and can
present in a manner which strays from a textbook presentation,
given the associated mortality a high index of clinical suspicion
is required and this case presentation serves as a gentle reminder for clinicians to not overlook ASR in their list of differential
diagnoses.
References
- Ciftci A, Colak E. Characteristics and surgical outcomes of patients with atraumatic splenic rupture. Journal of international
medical research. 2022; 50(2): 03000605221080875.
- Candinas D, Gloor B, Hostettler A, Renzulli P, Schoepfer M. Systematic review of atraumatic splenic rupture. British Journal of
Surgery. 2009; 96(10): 1114-1121.
- Clercq S, Guy s. Splenic rupture in community acquired pneumonia: A case report. International journal of surgical case reports.
2016; 29: 85-87.
- Chi W, Fang ZT, Lin C, Lin JL, Luo JW, et al. Splenic Artery Embolization and Splenectomy for Spontaneous Rupture of Splenic
Hemangioma and Its Imaging Features. Front Cardiovasc Med.
2022; 9: 925711.
- Christopher H, Jessica B, Robert P, Zayd A. Atraumatic Splenic
Rupture on Direct Oral Anticoagulation. J Community Hosp Intern Med Perspect. 2022; 12(5): 84-87.
- Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: A systematic
review. BMC Emerg Med. 2012; 12: 11.
- Levitt MA, Lieberman ME. Spontaneous rupture of the spleen: a
case report and literature review. Am J Emerg Med. 1989; 7(1):
28-31.