Introduction
The examination of pediatric patients frequently presents
limitations. We will probably find it more difficult to obtain information at a younger age of the patient. In addition, we must
keep in mind the context of the patient (if he has a delay in
maturation or any associated pathology that may make the examination more difficult). Because of this, sometimes we do not
achieve a precise diagnosis or a complete examination in the
consultation, and on certain occasions, we require an examination under sedation in the operating room.
When we perform an ophthalmological evaluation under
general anesthesia in a pediatric patient, we usually perform
sciascopy under cycloplegia, anterior segment examination
with a microscope or portable slit lamp, eye fundus examination (being able to collect images if a portable retino graph is
available), tonometry, ultrasound, biometry with axial length
measurements and keratometry in cases, for example, of congenital cataracts in which surgery is to be considered.
However, there are structures that we have not been able to
accurately evaluate on a regular basis due to not being able to
perform some complementary tests, which in consultation and
with collaborating patients is something routine, but not in the
pediatric age group [1]. Specifically, we are referring to optical
coherence tomography, it is a non‐contact and non‐invasive diagnostic imaging method that allows to obtain images of ocular issues in cross sections with very high-quality micrometric resolution [2], which provides additional information: In alterations
of the anterior segment that due to the existence of corneal
opacity, we cannot visualize directly, as in structures of the posterior segment [3].
In recent months, we have introduced, in cases that have required it, the use of a surgical Microscope with Integrated OCT
(MI‐OCT) to complete the examination, obtaining very useful
information to be able to establish a more precise diagnosis in
patients and, therefore, to be able to better define the therapeutic approach to follow, thus improving the visual prognosis
of these children [4]. In the work that we present here, we used
a group of patients to illustrate the advantages of this technique
and describe a new range of indications in both anterior and
posterior segments.
Case description
We present three pa ents who were examined at Hospital
Arruzafa (Córdoba, Spain) by examination under general anesthesia, using a microscope with integrated intraoperative OCT
(Zeiss Opmi Lumera 700). We have assessed whether the additional information obtained from this test had a significant impact on the therapeutic decision‐making process.
Zeiss Opmi Lumera 700 is a combination of opera ng microscope, OCT, surgical assistant system and fundus imaging system. It allows us to capture images by OCT in real me, intraoperatively. Currently, in their data sheet, they refer to its
usefulness mainly in surgical techniques, both for the anterior
pole (DSAEK, DALK, follow‐up of glaucoma surgery) and for the
posterior pole (peeling of the internal limiting membrane, macular holes, epiretinal membranes, renal detachment). However,
they do not highlight its use for exploration of these ocular
structures during an examination under general anesthesia.
Our pa ents were assessed under deep sedation. To obtain anterior segment images, we simply activate OCT mode and bring
the microscope head closer to the ocular surface until the desired plane is focused. For posterior segment imaging, we apply
viscoelastic to the ocular surface, we place in position the Resight device, which automatically activates the OCT mode on
the microscope. We bring it closer to the surface, placing it 1 or
2 mm from the cornea, and we focus on the pupil under mydriasis. From there, although we do not visualize the background, we focus with the microscope pedal until we visualize
and situate ourselves in the plane of the retina. Once in plane,
we can do the fine focus in the parameters of the screen.
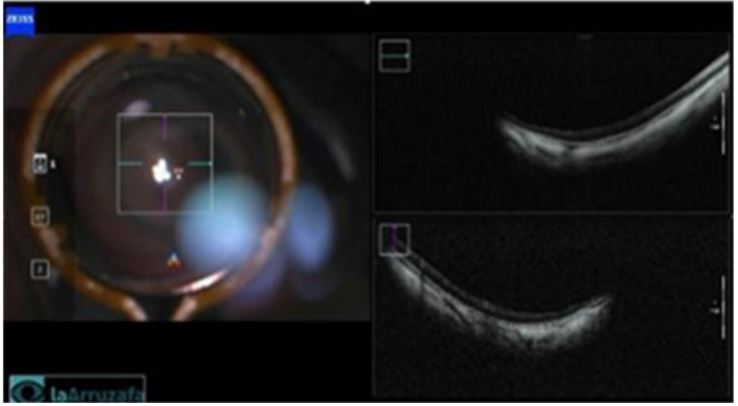
First case is a 2‐year‐old boy with esotropia since he was 6
months old, who comes to the clinic with prescribed glasses of
+4.00D for both eyes, which he does not tolerate. It does not
collaborate for taking visual acuity, nor for ophthalmological exploration, objectifying wide‐angle esotropia. It was decided to
explore in the operating room under sedation. We performed
sciascopy, with a result of PN‐12.00D in both eyes. No alterations were found in the anterior segment. The fundus of the eye
is very hypopigmented and we can see slightly pale papillae and
no foveal structure can be identified. It was decided to perform
intraoperative OCT, which determined the diagnosis of bilateral
foveal aplasia (Figure 1).
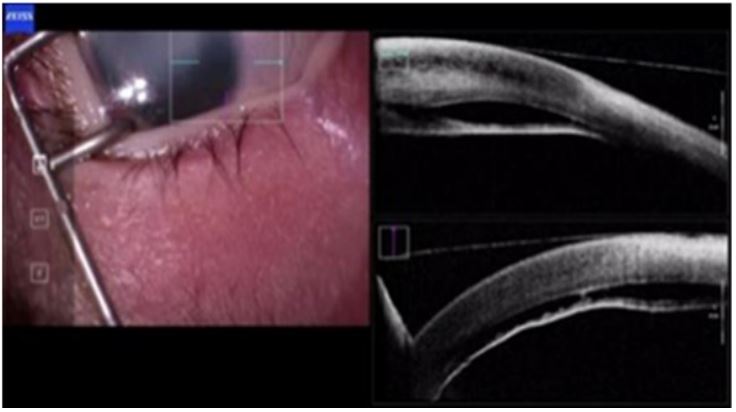
Second case is a two‐week‐old neonate with congenital corneal opacity in right eye, with no relevant family history, in
which slit‐lamp examination does not provide us with sufficient
information, although we can verify corneal opacity. It was decided to explore in the operating room under sedation. It is not
possible to perform sciascopy or assess the fundus due to media opacity. ECO is performed in which the applied retina and
vitreous cavity can be seen within normality. Left eye has no
alterations in the anterior or posterior segment. It was decided
to perform OCT of the anterior segment to be able to evaluate
the structures in detail and issue a possible diagnosis. OCT (Figure 2) reveals severe corneal opacity with increased corneal
thickness, edema and severe fibrosis, Descemet’s detachment,
and lens‐corneal contact at some points. Unstructured angle
with anterior synechiae and flattening of the anterior chamber.
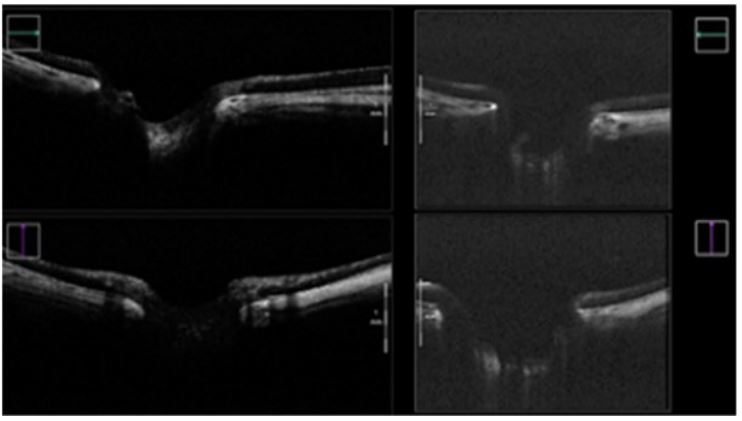
Third case is about a child with congenital glaucoma who un‐
derwent surgery twice in another center, who went to see an
optician in his city for detection of myopia. In the consulta on, it
is possible to obtain a VA of 0.1 in the right eye and it does not
help to obtain it in the left one. In the same way, it is not possible to perform sciascopy, nor take the IOP or perform an examination of the fundus. It was decided to explore in the operating room under sedation. Once sedated, sciascopy was
performed, with a result of PN ‐11.00D in right eye and ‐8.00D
in left eye. On exploration of the anterior segment, 14.5 mm
horizontal and vertical megalocorneas are observed. The IOP is
taken: 8 mmHg in AO. In the fundus, papillae with excavation
0.4 and 0.6 are observed, the excavation of le eye seems deeper. Intraoperative OCT (Figure 3) allows us to assess the degree
of papillary excavation and whether it is symmetrical.
Discussion
The ophthalmological examination of pediatric patients is
difficult and requires a lot of experience. Even so, there are cases in which the most experienced optometrist and the most expert ophthalmologist cannot perform their examinations on the
children in consultation. The ophthalmological examination of
these patients under sedation has clearly evolved with the incorporation of intraoperative OCT. Until its implementation, in
patients in whom the ophthalmologist had reduced visibility of
the anterior chamber of the eye, for example, due to congenital
corneal opacities, intraoperative imaging was limited to Ultrasonic Bio Microscopy [5] (UBM) and photographs. With BMU
we obtain a worse resolution and also if it is in the context of
surgery, the surgical procedure must be stopped to be able to
perform the exploration.
If we compare OCT devices integrated into surgical microscopes (MI‐OCT) with portable OCTs, there are all advantages:
Integration of intraoperative OCT control into the microscope
foot pedal and above all, the combination of a highly magnified
microscope image and high resolution OCT image.
Microscope‐integrated intraoperative OCT provides important information during the anesthetic examination of some
children. It brings the advantage that even with reduced visibility in the anterior chamber we can obtain high‐resolution images of anterior segment structures (including cornea, camera
angle, and lens). It allows us to evaluate alterations of the macula and the optic nerve in children who, due to their age or degree of collaboration, cannot perform an OCT in consultation. Is
intraoperative OCT essential for an ophthalmological examination of a pediatric patient under sedation? No, but it is very useful. Perhaps in the future its use will be standardized as part of
the pediatric examination under sedation.
Declarations
Patient consent: The family of the patients provided consent
to publish details of these cases.
Conflicts of interests: The Authors declare(s) that there is no
conflict of interest.
Funding: The authors received no financial support for the
research, authorship, and/or publica on of this are clear.
References
- Posarelli C, Sartini F, Casini G, Passani A, Toro MD, et al. What
Is the Impact of Intraoperative Microscope‐Integrated OCT in
Ophthalmic Surgery? Relevant Applications and Outcomes. A
Systema c Review. Journal of Clinical Medicine. 2020; 9: 1682.
- Benda T, Studený P. Intraoperative Optical Coherence Tomography ‐Available Technologies and Possibilities of Use. A Review.
Cesk Slov O almol. 2022; 78: 277286.
- Siebelmann S, Bachmann B, Horstmann J, Dietlein T, Lappas A,
et al. Mikroskopintegrierte intraoperative op sche Kohärenztomographie bei der Narkoseuntersuchung von pädiatrischen Patience. Microscope‐integrated intraoperative optical coherence
tomography in examination of pediatric pa ents under anesthesia. Ophthalmology. 2018; 115: 785‐792.
- Siebelmann S, Bachmann B, Lappas A, Dietlein T, Steven P, et al.
Intraoperative opsche Kohärenztomographie bei Narkoseuntersuchungen von Säuglingen und Kleinkindern. Intraoperative optical coherence tomography for examination of newborns and
infants under general anesthesia. Ophthalmology. 2016; 113:
651‐5.
- Siebelmann S, Hermann M, Dietlein T, Bachmann B, Steven P,
et al. Intraoperative Optical Coherence Tomography in Children
with Anterior Segment Anomalies. Ophthalmology. 2015; 122:
2582‐4.