Introduction
Lymphoma is a group of lymphoid malignancies that develop
from lymphocytes with two main types: Hodgkin lymphoma
(HL) and non-Hodgkin lymphoma. Lymphoma may present with
lymphadenopathy and classic systemic symptoms of fever, night
sweats and weight loss. Other less common symptoms can include fatigue, dyspnea, anorexia, pruritus and pain with alcohol
consumption. Less common symptoms can make it challenging
to determine appropriate investigations and achieve a timely
diagnosis.
Case report
A 32-year-old male developed left sided central chest pain
that started minutes after ingesting small amounts of alcohol
that would resolve over a short period of time or with continued alcohol consumption. The pain progressively worsened
over six months’ time and was absent with consumption of any
other solids or liquids. However, in a six-week time period a new
palpable firm two centimeter lesion developed between the
left anterior second and third ribs.
He reported mild fatigue, but denied any fevers, night sweats
or weight loss. His medical history was significant for Neurofibromatosis type 1. He was not on any medications, was a
never smoker and consumed daily light amounts of alcohol.
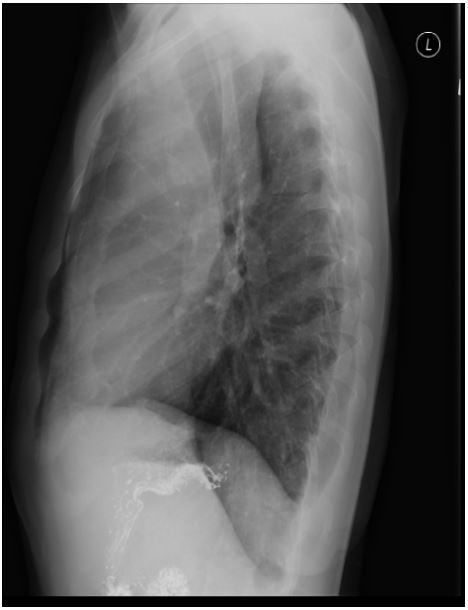
Initial testing included a normal barium swallow and chest xray showing an anterior mediastinal mass (Figure 1). Computed
tomography of the chest showed a bulky anterior mediastinal
mass (10.3x10.3x14.5 cm) with sternal/chest wall invasion and
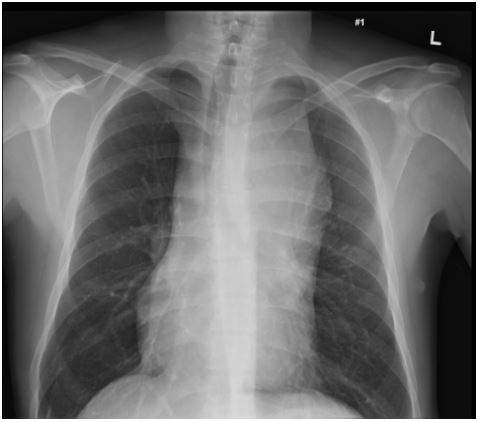
mediastinal lymphadenopathy. Positron emission tomography/
computed tomography (PET/CT) showed very non-homogeneous fluorodeoxyglucose (FDG) uptake internally with several
focal areas of very intense uptake (Figure 2). There was marked
metabolic activity within mediastinal, hilar, bilateral retro-pectoral, left supraclavicular and right axillary lymph nodes with increased metabolic activity in an area of manubrial lytic change.
Complete blood count, electrolytes, urea, creatinine, liver enzymes and lactate dehydrogenase were normal. Erythrocyte
sedimentation rate was elevated at 23 mm/hr. Viral hepatitis
and HIV testing was negative.
Core biopsy (16 gauge) of the mediastinal mass showed
polymorphous cellular infiltrate consisting of numerous small
mature lymphocytes, scattered histiocytes, eosinophils and occasional large atypical cells consistent with variants of Hodgkin and Reed-Sternberg (HRS) cells. Immunohistochemical
stains showed HRS cells positive for CD30, CD15 (small subset),
MUM1 and PAX5 (weak); and negative for CD45, CD20 and October 2. CD3 highlighted abundant small mature T-cells in the
background. An in-situ hybridization of EBV RNA (EBER) was
negative within HRS cells. The final diagnosis was Stage IVAEX
Classical HL nodular sclerosis subtype.
Treatment was with six cycles of Adriamycin, bleomycin,
vinblastine and dacarbazine (ABVD). Chest pain with alcohol
consumption and the mass between the ribs resolved after the
first treatment. Repeat PET/CT scan after the second ABVD cycle
showed considerable decrease in FDG avidity and size and of
the mass measuring 3.7x2.5 cm. Only a few foci of FDG uptake
persisted of similar intensity to background liver (Deauville category 3). Tumor extension into the left parasternal chest wall,
supraclavicular, axillary and mediastinal lymphadenopathy had
resolved. The manubrial abnormality had become more sclerotic and the FDG uptake had resolved, consistent with a healing
response. Bleomycin was removed for the remainder of treatment for long term risk reduction [1]. Consolidative radiation
was given (3000 cGy in 15 fractions) due to residual FDG foci
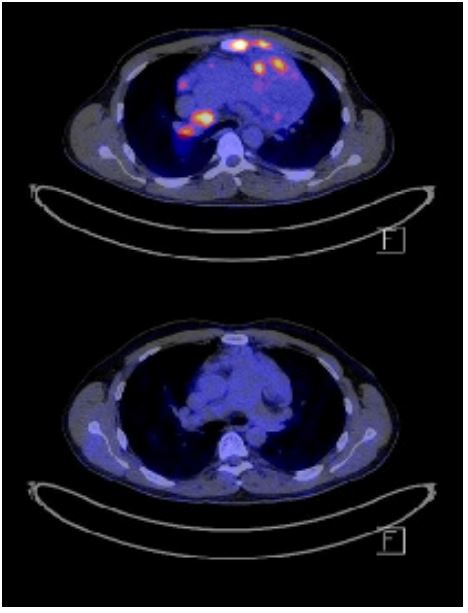
in the mass. Repeat PET/CT imaging shows complete metabolic
response to treatment (Figure 3). The patient’s disease remains
in remission four years after finishing treatment.
Comment
The incidence of alcohol related pain with HL was initially reported in 1950 [2] with an incidence of 1.5-5% of HL cases. The
differential diagnosis of alcohol-related pain or intolerance includes HL, carcinoid syndrome, alcohol dehydrogenase 2 mutations, other solid tumor malignancies and disulfiram reactions.
Alcohol related pain seems to be more common with HL nodular sclerotic subtype, affecting areas locally involved with HL.
Incidences of occurrence range from 7% patients with lymphadenopathy to 20% with bone involvement [3]. Treatment of HL
commonly results in resolution of alcohol related pain [4]. The
causes of alcohol-related pain in HL are unknown and are hypothesized to be related to vasodilation within the lymph node
causing capsular stretch or to acetic acid production in the tissues affected by HL [5,6]. PET/CT is a standard for evaluation,
staging and response assessment in lymphoma [7]. Early interim
PET-FDG uptake is a negative independent predictor of progression free survival and overall survival [8]. At this time there is no
strong evidence to support poorer outcomes for patients with
HL and alcohol related pain. In conclusion, lymphoma should be a diagnostic consideration with symptoms of alcohol related
pain. Resolution of alcohol related pain indicates treatment response which can be correlated with radiological imaging. PET/
CT imaging is useful in lymphoma treatment planning and in
determining treatment response.
References
- Johnson P, Federico M, Kirkwood A, et al. Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s lymphoma. N Engl J Med. 2016; 374: 2419-29.
- Hoster HA. Hodgkin’s disease. Am J Roentgenol Radium Ther. 1950; 64(6): 913-8.
- Bobrove AM. Alcohol-related pain in Hodgkin’s disease. West J Med. 1983; 138: 874-5.
- Atkinson K, Austin DE, McElwain TJ, Peckham MJ. Alcohol pain in Hodgkin’s disease. Cancer. 1976; 37(2): 895-9.
- Brewin TB. Alcohol intolerance in neoplastic disease. Br Med J. 1966; 2(5511): 437-441.
- Banerjee D. Recent advances in the pathobiology of Hodgkin’s lymphoma: potential impact on diagnostic, predictive, and therapeutic strategies. Adv Hematol. 2011: 439456.
- Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014; 32(27): 3059-3068.
- Mikhaeel NG, Hutchings M, Fields PA, O’Doherty MJ, Timothy AR. FDG-PET after two to three cycles of chemotherapy predicts progression-free and overall survival in high-grade Non-Hodgkin lymphoma. Ann Oncol. 2005; 16(9): 1514-23.