Introduction
Hip fractures are one of the most common traumatic injuries in the geriatric population, defined as those aged 65 years
and older. Beyond the immediate implications of the injury itself, these fractures usher in heightened mortality rates, steep
functional declines, and substantial economic burdens on
healthcare systems and society at large [1,2]. As age advances,
the occurrence of these fractures is expected to rise, mirroring
the global trend where the elderly population is the fastest expanding demographic. The incidence of hip fractures in Iceland
aligns closely with figures reported from other Scandinavian nations, as documented in prior research in Iceland [3]. While the
emphasis in managing hip fractures is the rapid restoration of
mobility, surgical interventions, the cornerstone of treatment,
are not without pitfalls. The procedures intended to repair hip
fractures sometimes culminate in severe complications [4-6].
Among these complications is mechanical failure or osteosynthesis failure which frequently necessitates subsequent reoperations [7,8]. Different reasons for mechanical failure have been
studied extensively but most often focusing either on Femoral
Neck Fracture (FNF) or the trochanteric fractures [9-14]. Moreover, there’s a paucity of data specifically addressing mechanical
failures post-hip surgeries in Iceland. Our study aimed to comprehensively document instances of mechanical failure following hip fracture surgeries at Landspítalinn University Hospital in
Iceland between 2013 and 2018. Simultaneously, we sought to
investigate whether specific deficiencies in the applied surgical
techniques might contribute to the occurrence of mechanical
failures. Thus, our research question emerged: ‘Are there identifiable deficiencies in the surgical techniques applied during hip
fracture surgeries at Landspítalinn University Hospital in Iceland
between 2013 and 2018 that are associated with an increased
risk of mechanical failure?’ By delving into this question, we aim
to provide valuable insights that not only enhance our understanding of hip fracture complications but also offer guidance
for refining surgical practices to optimize patient outcomes.
Material and methods
Study design: This was a retrospective non-comparative cohort study conducted at the Orthopedic department in Landspítalinn University Hospital in Iceland.
Patient selection: All patients who underwent surgery after
a hip fracture in the period 01.01.2013-31.12.2018 were eligible for inclusion. We excluded subjects who did not have a reoperation, had a reoperation for reasons other than mechanical
failure such as wound revision or infection or had a high energy
fracture.
Data collection: Clinical data were collected from electronic
medical records. Pre-, post-operative and follow-up x-rays were
reviewed. Information on surgical techniques and implant types
were collected from surgical reports.
Radiographic analysis: Radiological analysis was done by the
author in Agfa Enterprise Imaging Program. Factors as the cause
of fixation failure which were classified into two primary groups
based on the time of occurrence: failures that happened before
6 months and those that occurred after 6 months. If the failure
occurred after 6 months, it was labeled as non-union. The specific subgroups identified in our analysis can be found in Table 1.
Table 1: Classification of fixation failure causes.
| Causes |
in |
| Aseptic Loosening |
1 |
| Axial/Valgus/Varus Collapse |
12 |
| Caput Necrosis |
13 |
| Cut Out |
13 |
| Dislocation >= 3 |
11 |
| Fracture near Osteosynthesis, Non-Traumatic |
1 |
| Fracture of Osteosynthesis |
4 |
| Nonunion |
6 |
| Nonunion and Axial/Valgus/Varus Collapse |
10 |
| Nonunion and Cut Out |
3 |
| Nonunion and Fracture of Osteosynthesis |
3 |
| Rotational Instability |
1 |
Intertrochanteric and subtrochanteric fractures were classified according to AO/OTA classification into A1, A2 and A3.
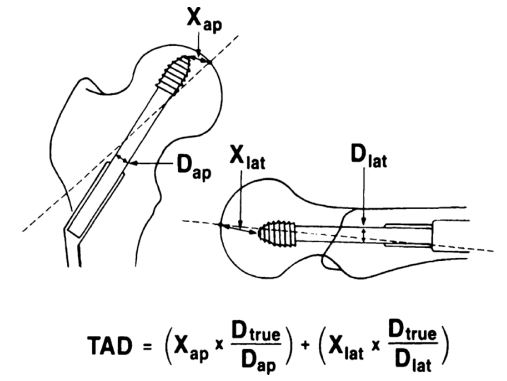
Baumgartner’s method, as shown in Figure 1, was employed to
evaluate the Tip Apex Distance (TAD) [14] for all the fractures
that were treated with Dynamic Hip Screw (DHS) or Intramedullary Nail (IMN).
The assessment of reduction quality was based on Baumgartner’s three grade scale evaluating two criteria on Antero-Posterior (AP) and lateral views [14]. The first criterion focuses on the
alignment, specifically the cervicodiaphyseal angle ranging from
120° to 135° on the AP view and an angulation of less than 20°
on the lateral view. The second criterion examines the displacement, with the requirement of less than 4 mm between each
fragment in both the AP and lateral views. The reduction was
classified as good if both criteria were met, if only one criterion
was met, the reduction was considered acceptable. However,
if neither criterion was met, the reduction was categorized as
poor. To estimate the position of the lag screw within the femoral head we used Parker’s ratio index [15]. Femoral neck fractures were classified as displaced (Garden III and IV) and undisplaced (Garden I and II) which has shown better inter-observer
reliability [16]. The Hansson pin system from Swemac is utilized
for the management of undisplaced femoral neck fractures at
Landspítalinn University Hospital [17]. We evaluated the quality
of fracture reduction and the accuracy of pin placement by applying criteria established in prior studies conducted in Norway
[18-20]. Detailed description of the criteria can be seen below.
When assessing pin placement and reduction, bear in mind that
the x-ray images used for the analysis weren’t standardized in
terms of hip rotation.
a. Fracture reduction: In the AP view, the fracture should
show no varus or up to 15° valgus angulation and less than 2
mm displacement. In the lateral view, the angulation should be
less than 20° ventrally or 10° dorsally, and displacement should
be less than 2 mm. A score system was used, where 3 points
indicated that all criteria were met, 2 points indicated that one
criterion was not satisfied, and 1 point indicated that two criteria were not satisfied. Points were assigned for both AP and
lateral views, with a maximum score of 6 points.
b. Pin placement: In the AP view, the caudal pin should
align along the calcar, the distance between pins should be
maximized within the anatomy of the femoral neck, both pins
should run parallel to the femoral neck, and both pins should
be inserted into the subchondral bone within 5 mm of the cartilage. In the lateral view, no pins should be positioned in the
anterior third of the femoral head, and one point was deducted
for each pin placed in this region. Similarly, a score system was
used, with 3 points indicating that all criteria were satisfied, 2
points indicating that one criterion was not met, and 1 point
indicating that two or more criteria were not fulfilled. Points were assigned for both AP and lateral views, with a maximum
score of 6 points. Displaced femoral neck fractures are treated
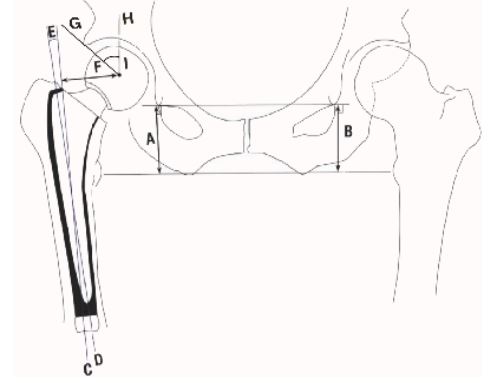
with cemented hemi prosthesis or total hip prosthesis depending on patient factors. In this study we documented Leg Length
Discrepancy (LLD), Femoral Offset, Fem-Stem Alignment (FSA)
and Wibergs angle or Center-Edge Angle (CEA). A diagrammatic
representation of the measurement parameters can be seen
Figure 2.
Statistical analysis: Statistical analysis was conducted using
R Studio (2023.06.0). Descriptive statistics were used to summarize patient characteristics and surgical techniques.
Ethical considerations: The study was approved by the Ethical Committee and the Scientific Research Committee of health
research in the health department at Landspítali. Informed consent was waived due to the retrospective nature of the study.
Patient confidentiality was maintained throughout the study by
using anonymized data.
Results
A total of 1876 hip fractures were identified and reviewed.
After exclusion criteria were applied (patients who did not have
a reoperation, had a reoperation for reasons other than a failed
internal fixation such as wound revision or infection or had a
high energy fracture), 78 surgeries on 75 patients were included
in the final analysis with a mean age of 76 years, ranging from
38 to 96 years old. Majority of the reoperations were done on
females, or 62% (48/78). The mean ASA score before surgery
was 2.5, 45% (35/72) of the patients were ASA 3, 40% (31/72)
ASA 2, 5% (4/72) ASA 4, 3% (2/78) ASA 1 but in 8% (6/78) there
was no ASA score recorded. The mean time between the initial
surgery and reoperation was 241 days but the median was 162
days, with a minimum of 7 days and a maximum of 1264 days.
The surgeries were categorized based on the original surgical
procedure performed, majority were Hansson 40% (31/78), followed by DHS (Synthes) 30% (23/78), IMN (Gamma 3 Stryker
and PFN Synthes) 15% (12/78), bipolar hemi prosthesis (MS30
Zimmer) 12% (9/78), and THA (Taperloc/Exceed Zimmer) 4%
(3/78). The causes of fixation failure can be seen in summarized
in Table 1.
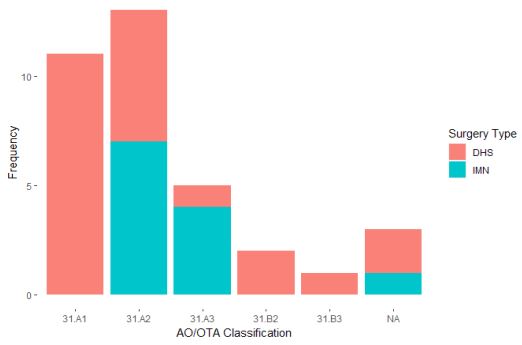
Trochanteric fractures: In Figure 3 the classification details
are presented according to the surgery performed. Mean TAD
was 27.7 mm, ranging from 6 to 46mm, in 60% (21/35) of the
surgeries TAD was above 25mm. The assessment of reduction
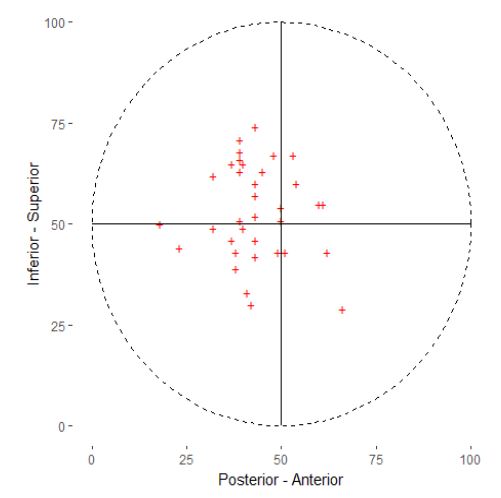
quality could not be carried out as intended due to the substantial number of instances where measurements on lateral fluoroscopy were unattainable due to poor image quality. The average Parkers ratio on the AP view was 53.2, with a range of 29 to
74. On the lateral view, the mean ratio was 43.6, ranging from
18 to 66. The distribution of Parkers ratio is depicted in Figure 4.
Femoral neck fractures: The majority of the femoral neck
fractures were treated with the Hansson pin system or 72%
(31/43), 21% (9/43) were treated with hemi prosthesis and 7%
(3/43) were treated with total prosthesis. Of the 31 fractures
who were treated with the Hansson pin system 55% (17/31)
were displaced fractures, 42% (13/31) undisplaced and 1 fracture was unclassifiable due to lack of preoperative radiograph.
In almost half of the cases or 42% (13/31) the reduction quality
in internal fixation achieved a score of 6 points, indicating no reduction of points. Meanwhile, 26% (8/31) scored 5 points, 13% (4/31) scored 4 points, and a minority of 16% (5/31) recorded 4
or fewer points. In total there was a reduction of 35 points. The
most prevalent cause for point reduction was a 2 mm displacement observed on the AP view, accounting for 31% (11/35) of
the reduced points. The next most common cause, comprising
20% (7/35) of the reductions, was a 2mm displacement seen
on the lateral view. Regarding pin placement, in more than half
or 61% (19/31) of the cases there is a reduction of at least one
point. Scores of 6 points were seen in 39% (12/31) of cases, 5
points in 36% (11/31), and 4 points in 23% (7/31). A cumulative
reduction of 25 points was observed, with 64% (16 out of 25)
being due to the pin spacing not fully utilizing the anatomical
breadth of the femoral neck. The second most frequent reason
for reduction, accounting for 28% (7/25) of the reduced points,
was the placement of one or more pins in the anterior third of
the femoral head. When analyzing hip prostheses, encompassing both hemi and total prostheses, it was observed that the
majority displayed varus alignment, constituting 75% (9/12) of
the cases. However, only one prosthesis deviated more than 5
degrees from the neutral position, exhibiting 8.6 degrees of varus. Among the prostheses, only two had a shorter offset compared to the unaffected side, measuring -11 mm and -12 mm.
The mean offset was 12 mm, with a median of 8.2 mm, ranging
from -12 mm to 20 mm. In terms of CEA, the average measurement was 30 degrees, ranging from 26 to 40 degrees. Furthermore, the mean LLD was 2.3 mm, with a range from 0mm to 5
mm longer.
Discussion
In this retrospective analysis, we conducted a comprehensive review of all surgeries following femoral neck and intertrochanteric fractures. For the subset that underwent reoperation,
we performed an evaluative grading of the implant positioning. We will discuss relevant outcomes for each fracture type
and surgery type, starting with general factors and then each
measuring factor. The average time between the initial surgery
and reoperation was 264 days, with a median of 162 days. Four
outlier cases were observed, ranging from 834 to 1264 days between the surgeries. Three of these cases involved caput necrosis, with patients reporting pain within two years of surgery. The
remaining case had a hemi prosthesis that persistently dislocating post-surgery.
Femoral neck fractures: The conventional method of closed
reduction and internal fixation for displaced femoral neck fractures has long been associated with a significant risk of reoperation [9,22-24]. A total of 31 subjects who received Hansson nails
required reoperation. The fact that 42% (13/31) of the patients
requiring reoperation had initially presented with a displaced
fracture underlines this concern. This points towards a possible
over-reliance on internal fixation in instances where arthroplasty would have been a more fitting treatment choice. In grading
reduction and pin placement quality, we used previously developed criteria which can be seen in the methods above. Almost
half of the cases or 42% (13/31) the reduction achieved a score
of 6 points, indicating no reduction of points. However, an apparent discrepancy arises as 58% (18/31) of the fractures were
initially categorized as undisplaced. This divergence results
from the fact that the Garden criteria, used for classifying fractures into displaced or undisplaced, only considers the AP view,
whereas our reduction criteria take both the AP and L views
into account. Previous comparable studies have shown an association between quality of reduction and reoperation or failure of treatment [13,18,19,25]. In our work, we found that 58% (18/31) of reductions saw at least a one-point decrease. This
underlines the critical need for precision during femoral neck
fracture reduction. Alternatively, as we’ve suggested before,
opting for arthroplasty over internal fixation in displaced femoral neck fractures. Regarding pin placement, only 39% (12/31)
had no reduction of points and the most common reduction of
points was due to the pin spacing not fully utilizing the anatomical breadth of the femoral neck. The influence of pin placement
on treatment outcomes remains ambiguous, as highlighted by
the conflicting results from previous studies [13,18,19].
Arthroplasty: In our cohort, only one arthroplasty was performed using the anterolateral approach, with the remaining
utilizing the posterolateral approach, reflecting surgeon preference. The use of the anterolateral approach in Iceland has since
2018 seen a considerable increase in contemporary arthroplasty treatments for femoral neck fractures. For arthroplasties
necessitating reoperation, the majority or 75% (9/12) exhibited
a varus alignment, with just one hip exceeding 5 degrees in
varus. The mean varus deviation from neutral was 2.5 degrees.
This suggests that the femoral stem alignment in femoral neck
fractures treated with arthroplasty and later requiring reoperation was generally acceptable. Past research has identified an
association between reduced femoral offset, compared to the
naïve hip, and dislocations [26-29] although others show no
correlation [12,30]. In our study, only 17% (two hips) demonstrated a femoral offset less than the native hip (-11 mm and
-12 mm), with a mean offset of 8.2 mm above the native hip.
Decreased CEA has been correlated to increased risk of dislocation [12,26,27,30,31], our average CEA was 30, ranging from 26-
40 degrees. Furthermore, none of the arthroplasties resulted in
a negative leg length discrepancy, with an average increase of
2.3 mm and a maximum of 5 mm. From these observations, we
infer that patient-related factors may have a more significant
role in arthroplasty failure than surgical factors, as per the parameters we evaluated.
Trochanteric fractures: A total of 35 failures were observed
in trochanteric fractures: 23 with DHS, 10 with gamma nails, and
2 with PFN nails. These fractures were classified using the AO/
OTA 2018 criteria. The DHS, with the most specific indications
among the three procedures, is mainly recommended for 31.A
fractures (DHS surgical manual). However, it can be adapted for
31.B2/3 by incorporating an anti-rotational screw [32] and for
31.A2/3 with a trochanteric stabilization plate [33], as outlined
in the DHS surgical manual. Even so, some research recommend IMN for unstable intertrochanteric fractures as Kregor
showed in his review [34]. Figure 3 depicts the application of
DHS and PFN for each fracture type. We noted the use of DHS +
trochanteric stabilization plate for A3 fractures and DHS + antirotational screw for B2 and B3 fractures. Our data suggests an
excessive application of DHS for A2 fractures that later required
reoperation, underscoring the need for thorough preoperative
planning.
TAD: The Tip Apex Distance (TAD) plays a pivotal role in predicting the outcome and stability of fixations in trochanteric
fractures [14,35,36]. In our study, the average TAD observed
for both the DHS and IMN stood at 27.7 mm, covering a broad
range from 6 mm to a relatively high 46 mm. Notably, a significant 60% (21/35) of the surgeries demonstrated a TAD exceeding the 25mm threshold. This finding is crucial, given that
numerous studies have highlighted the 25 mm mark as a critical
threshold for predicting screw cut-out and post-operative complications. The prominence of TAD measurements exceeding this threshold in our sample suggests potential areas for optimization in our surgical techniques.
Position of the lag screw: Lag screw positioning within the
femoral head is important for optimal outcomes following fracture fixation. The prevailing recommendation from many studies is a central/central lag screw orientation in AP and L views
[10,11,15,35], yet some studies argues an inferior placement
might be preferable to the central one [37-39]. The positioning
of the lag screw in our study appears to be acceptable considering these are the surgeries that went into failure, showing a
minor superior bias with a Parker’s ratio of 53.2 and a slight posterior alignment, evidenced by a Parker’s ratio of 43.6. As mentioned in our results we set out to qualify the intraoperative
reduction quality but the measurements on lateral fluoroscopy
were unattainable due to poor quality. This can be prevented by
making sure to include the whole osteosynthesis, caput femoris, greater trochanter and the femoral shaft on the lateral fluoroscopy.
Conclusion
Hip fractures, particularly in the geriatric population, pose
significant medical and societal challenges. While surgical intervention remains the cornerstone of management to expedite mobility, its potential complications, including mechanical
or osteosynthesis failures, necessitate keen clinical vigilance.
Through our study of surgeries performed at Landspítalinn University Hospital in Iceland between 2013 and 2018, we aimed
to shed light on the underlying reasons for reoperations, with
a focus on potential deficiencies in surgical techniques. Our research aligns with the prevailing agreement in existing literature that emphasizes the preference for hemiprosthesis over
ORIF in treating displaced FNF. Additionally, our findings reveal
a notable propensity for employing DHS fixation in cases of
31. A2 intertrochanteric fractures during the period spanning
2013-2018. Furthermore, we observed that the TAD exceeded
the critical 25 mm threshold in 60% of our cases, a significant
predictor of screw cut-out. These outcomes underscore the
importance of meticulous surgical techniques and a thorough
understanding of the appropriate surgical interventions for specific fracture types. In the constantly evolving field of orthopedic surgery, it is crucial to continually assess and refine our techniques, ensuring optimal outcomes for patients and reducing
the burden on healthcare systems.
Conflicts of interest: We have no conflicts to disclose.
References
- Collaborators, GBDF. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021; 2: 580-592.
- Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, et al. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos Int. 2017; 28: 2791-2800.
- Siggeirsdottir K, Aspelund T, Jonsson BY, Mogensen B, Gudmundsson EF, et al. Epidemiology of fractures in Iceland and secular trends in major osteoporotic fractures 1989-2008. Osteoporos Int. 2014; 25: 211-219.
- Goh EL, Lerner RG, Achten J, Parsons N, Griffin XL, et al. Complications following hip fracture: Results from the World Hip Trauma Evaluation cohort study. Injury. 2020; 51: 1331-1336.
- Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: Prospective observational cohort study. BMJ. 2005; 331: 1374.
- Flikweert ER, Wendt KW, Diercks RL, Izaks GJ, Landsheer D, et al. Complications after hip fracture surgery: Are they preventable? Eur J Trauma Emerg Surg. 2018; 44: 573-580.
- Gjertsen JE, Engesaeter LB, Furnes O, Havelin LI, Steindal K, et al. The Norwegian Hip Fracture Register: Experiences after the first 2 years and 15,576 reported operations. Acta Orthop. 2008; 79: 583-593.
- Gromov K, Brix M, Kallemose T, Troelsen A. Early results and future challenges of the Danish Fracture Database. Dan Med J. 2014; 61: 4851.
- Bhandari M, Devereaux PJ, Swiontkowski MF, bremskey W, Koval, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003; 85: 1673-1681.
- Bojan AJ, Beimel C, Taglang G, Collin D, Ekholm C, et al. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013; 14: 1.
- Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, et al. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990; 72: 26-31.
- Fakler JKM, Rositzka M, Schopow N, Roth A, Zajonz D, et al. Factors associated with dislocation after bipolar hemiarthroplasty through an (antero-)lateral approach in elderly patients with a femoral neck fracture: A retrospective cohort study with a nested case-control subanalysis of radiographic parameters. Eur J Trauma Emerg Surg. 2022; 48: 3981-3987.
- Heetveld MJ, Raaymakers EL, Luitse JS, Gouma DJ. Rating of internal fixation and clinical outcome in displaced femoral neck fractures: A prospective multicenter study. Clin Orthop Relat Res. 2007; 454: 207-213.
- Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77: 1058-1064.
- Parker MJ. Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg Br. 1992; 74: 625.
- Van Embden D, Rhemrev SJ, Genelin F, Meylaerts SA, Roukema GR. The reliability of a simplified Garden classification for intracapsular hip fractures. Orthop Traumatol Surg Res. 2012; 98: 405-408.
- Stromqvist B, Hansson LL, Nilsson LT, Thorngren KG. Hook-pin fixation in femoral neck fractures. A two-year follow-up study of 300 cases. Clin Orthop Relat Res. 1987; 58-62.
- Hoelsbrekken SE, Opsahl JH, Stiris M, Paulsrud O, Stromsoe K. Failed internal fixation of femoral neck fractures. Tidsskr Nor Laegeforen. 2012; 132: 1343-1347.
- Lykke N, Lerud PJ, Stromsoe K, Thorngren KG. Fixation of fractures of the femoral neck. A prospective, randomised trial of three Ullevaal hip screws versus two Hansson hook-pins. J Bone Joint Surg Br. 2003; 85: 426-430.
- Mjorud J, Skaro O, Solhaug JH, Thorngren KG. A randomised study in all cervical hip fractures osteosynthesis with Hansson hook-pins versus AO-screws in 199 consecutive patients followed for two years. Injury. 2006; 37: 768-777.
- James HK, Pattison GTR, Griffin J, Fisher JD, Griffin DR. Assessment of technical skill in hip fracture surgery using the postoperative radiograph: Pilot development and validation of a final product analysis core outcome set. Bone Jt Open. 2020; 1: 594-604.
- Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br. 2010; 92: 406-412.
- Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006; 77: 359-367.
- Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006; CD001708.
- Kalsbeek JH, van Donkelaar MF, Krijnen P, Roerdink WH, de Groot R, et al. What makes fixation of femoral neck fractures fail?. A systematic review and meta-analysis of risk factors. Injury. 2023; 54: 652-660.
- Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, et al. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty. 2009; 24: 768-774.
- Madanat R, Makinen TJ, Ovaska MT, Soiva M, Vahlberg T, et al. Dislocation of hip hemiarthroplasty following posterolateral surgical approach: A nested case-control study. Int Orthop. 2012; 36: 935-940.
- Mukka S, Lindqvist J, Peyda S, Broden C, Mahmood S, et al. Dislocation of bipolar hip hemiarthroplasty through a postero-lateral approach for femoral neck fractures: A cohort study. Int Orthop. 2015; 39: 1277-1282.
- Forde B, Engeln K, Bedair H, Bene N, Talmo C, et al. Restoring femoral offset is the most important technical factor in preventing total hip arthroplasty dislocation. J Orthop. 2018; 15: 131-133.
- Zhang Y, Yao Z, Shi P, Wang C, Liu J, et al. Morphological risk factors associated with dislocation after bipolar hemiarthroplasty of the hip in patients with femoral neck fractures-a nested casecontrol study. J Orthop Surg Res. 2019; 14: 395.
- Kizkapan TB, Misir A, Uzun E, Oguzkaya S, Ozcamdalli M. Factors affecting dislocation after bipolar hemiarthroplasty in patients with femoral neck fracture. Injury. 2020; 51: 663-669.
- Dekhne MS, Thomas HM, Haider T, Mortensen S, et al. Treatment and outcomes of basicervical femoral neck fractures: A systematic review. J Orthop Surg (Hong Kong). 2021; 29: 23094990211003344.
- Selim A, Ponugoti N, Naqvi AZ, Magill H. Cephalo-medullary nailing versus dynamic hip screw with trochanteric stabilisation plate for the treatment of unstable per-trochanteric hip fractures: A meta-analysis. J Orthop Surg Res. 2021; 16: 47.
- Kregor, PJ, Obremskey WT, Kreder HJ, Swiontkowski MF. Evidence-Based Orthopaedic Trauma Working, G. Unstable pertrochanteric femoral fractures. J Orthop Trauma. 2005; 19: 63-66.
- Morvan A, Boddaert J, Cohen Bittan J, Picard H, Pascal Mousselard H, et al. Risk factors for cut out after internal fixation of trochanteric fractures in elderly subjects. Orthop Traumatol Surg Res. 2018; 104: 1183-1187.
- Rubio Avila J, Madden K, Simunovic N, Bhndari M. Tip to apex distance in femoral intertrochanteric fractures: A systematic review. J Orthop Sci. 2013; 18: 592-598.
- Kuzyk PR, Zdero R, Shah S, Olsen M, Waddell JP, et al. Femoral head lag screw position for cephalomedullary nails: A biomechanical analysis. J Orthop Trauma. 2012; 26: 414-421.
- Goffin JM, Pankaj P, Simpson AH. The importance of lag screw position for the stabilization of trochanteric fractures with a sliding hip screw: A subject-specific finite element study. J Orthop Res. 2013; 31: 596-600.
- Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir O, et al. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J. 2014; 96-B: 1029-1034.